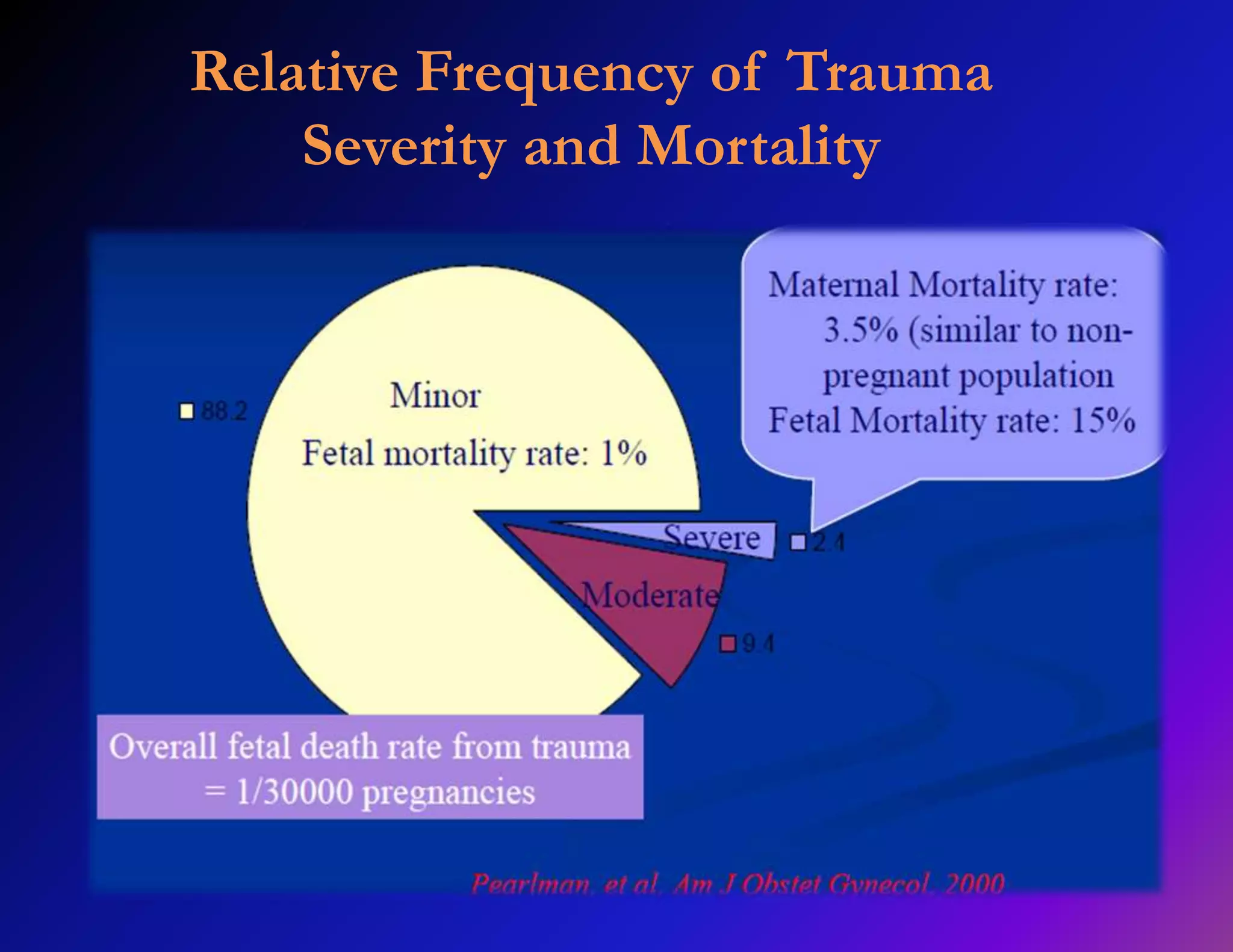
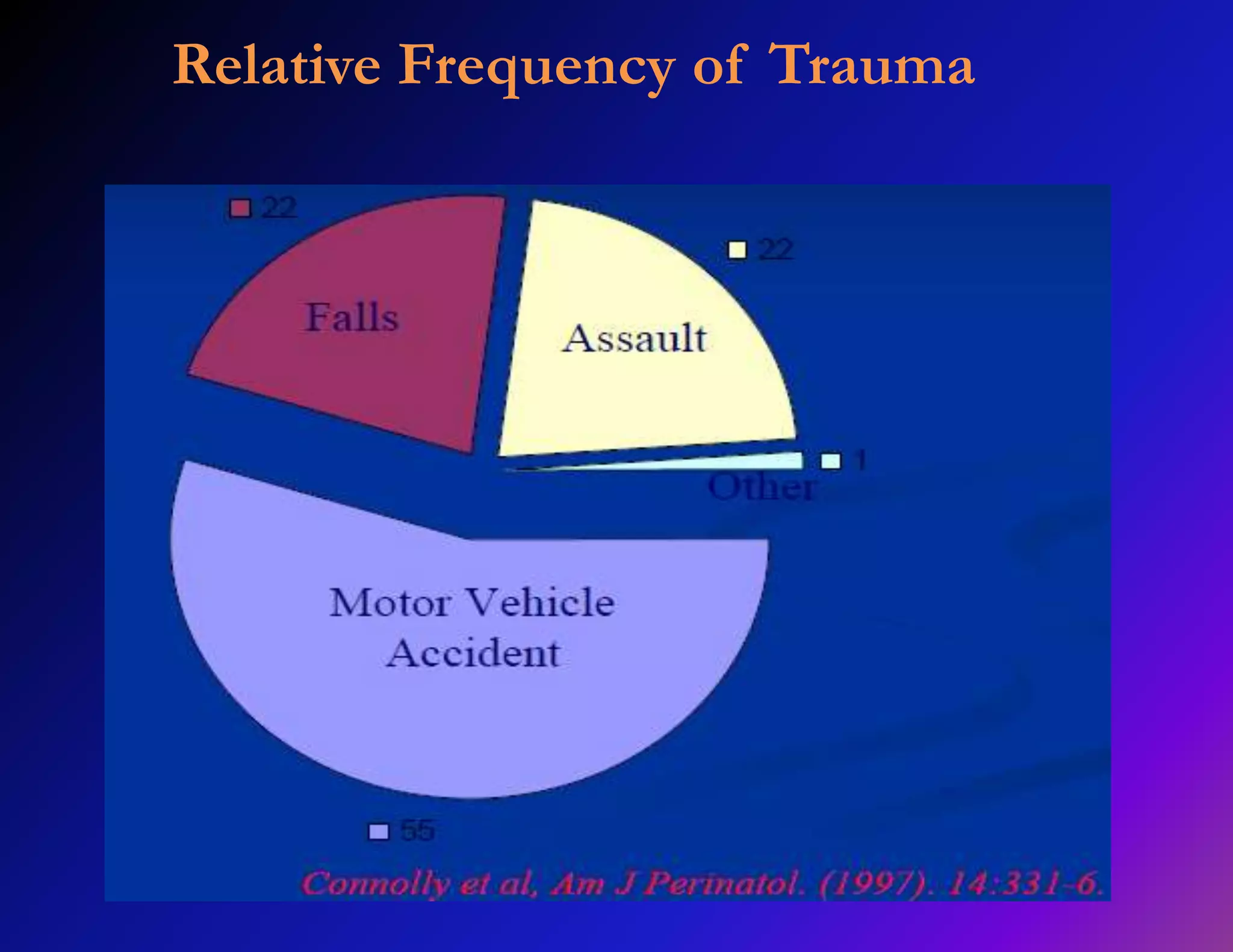
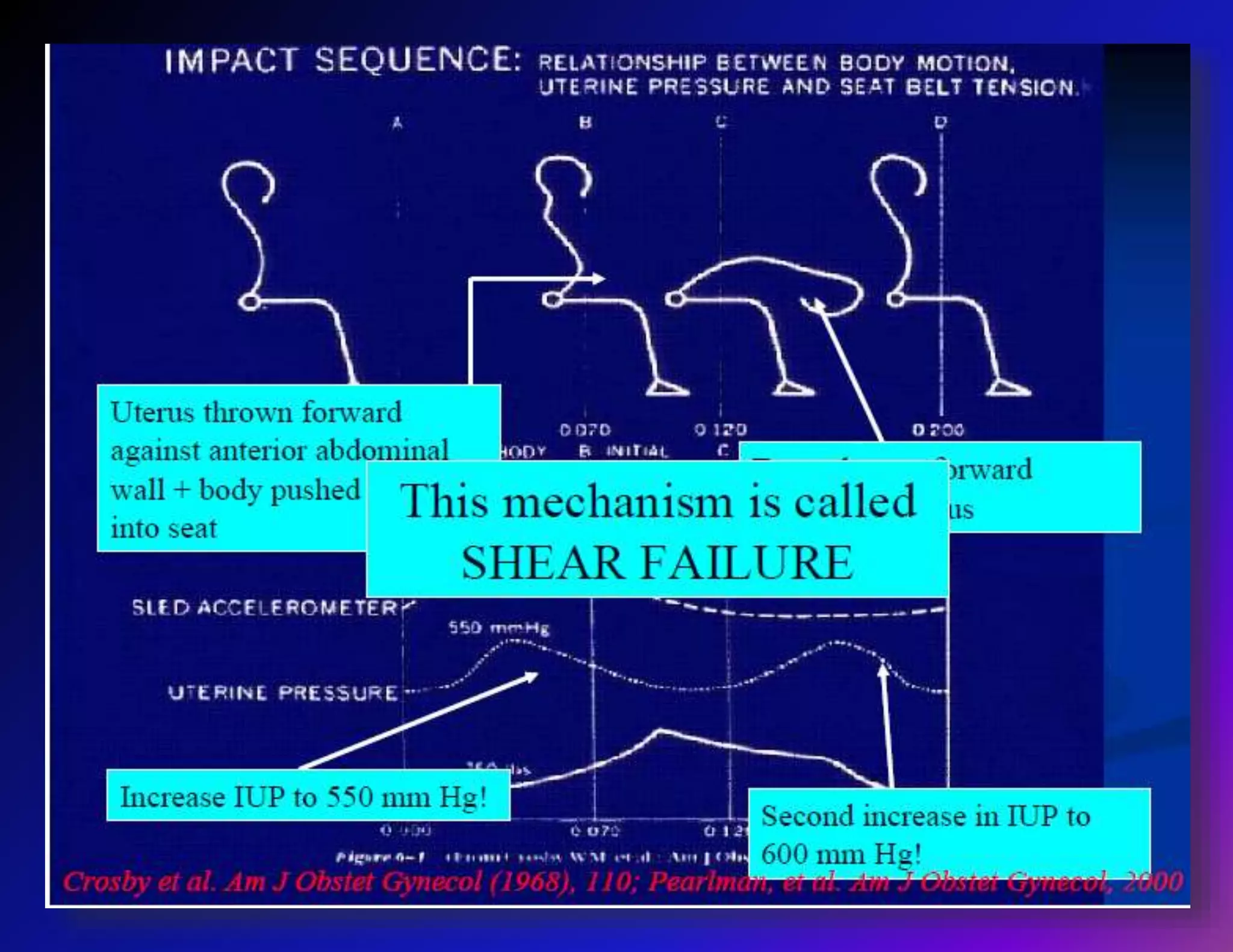
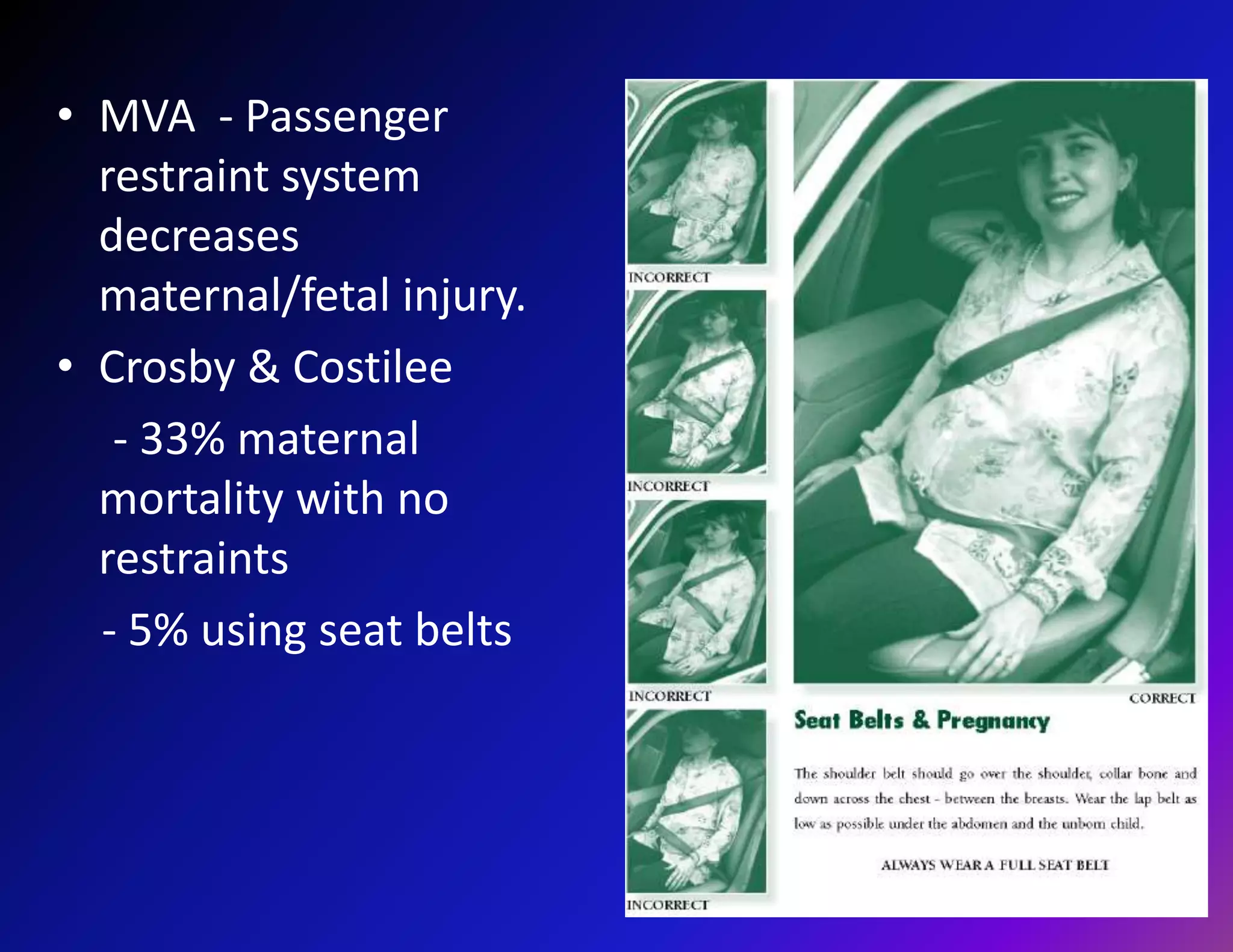
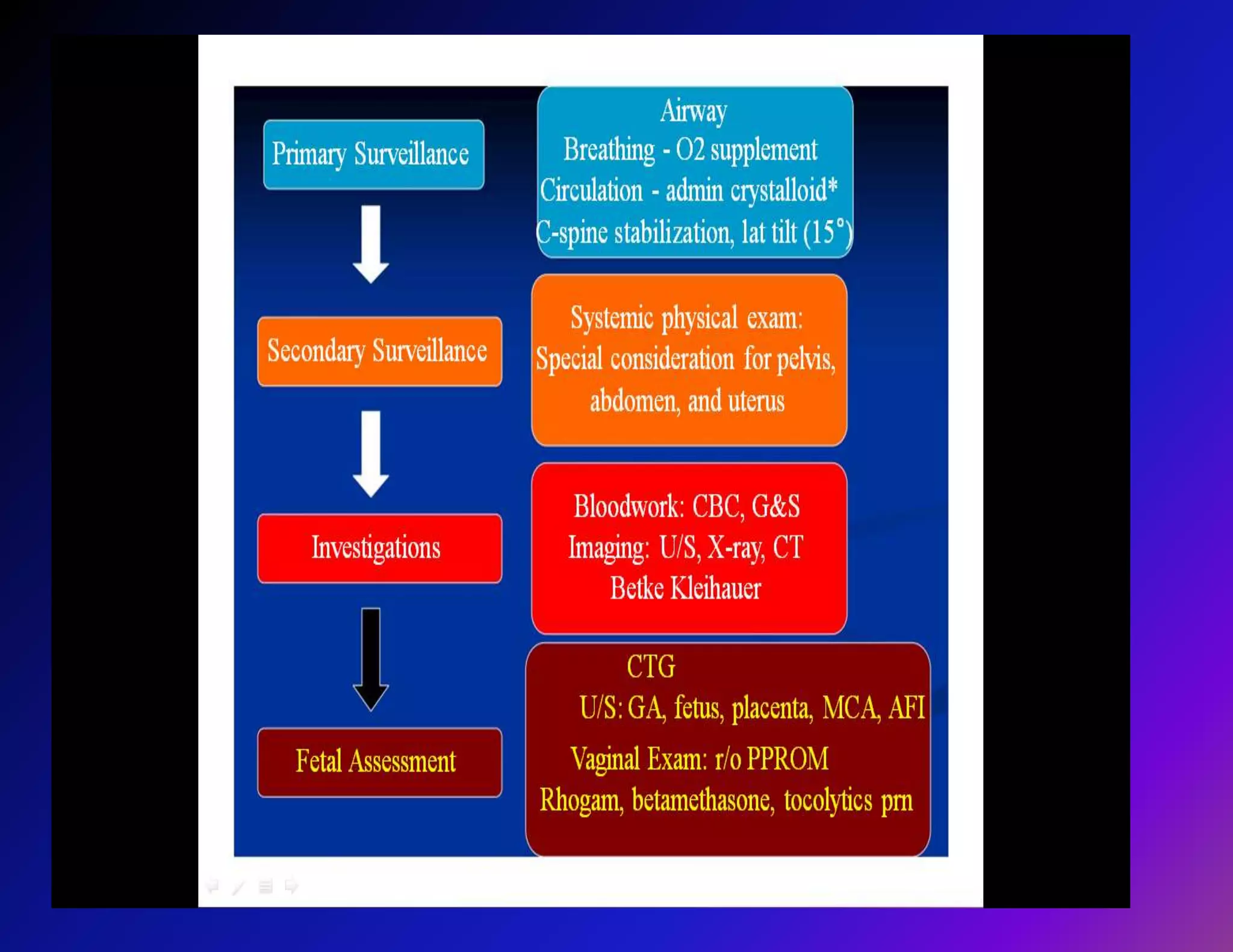
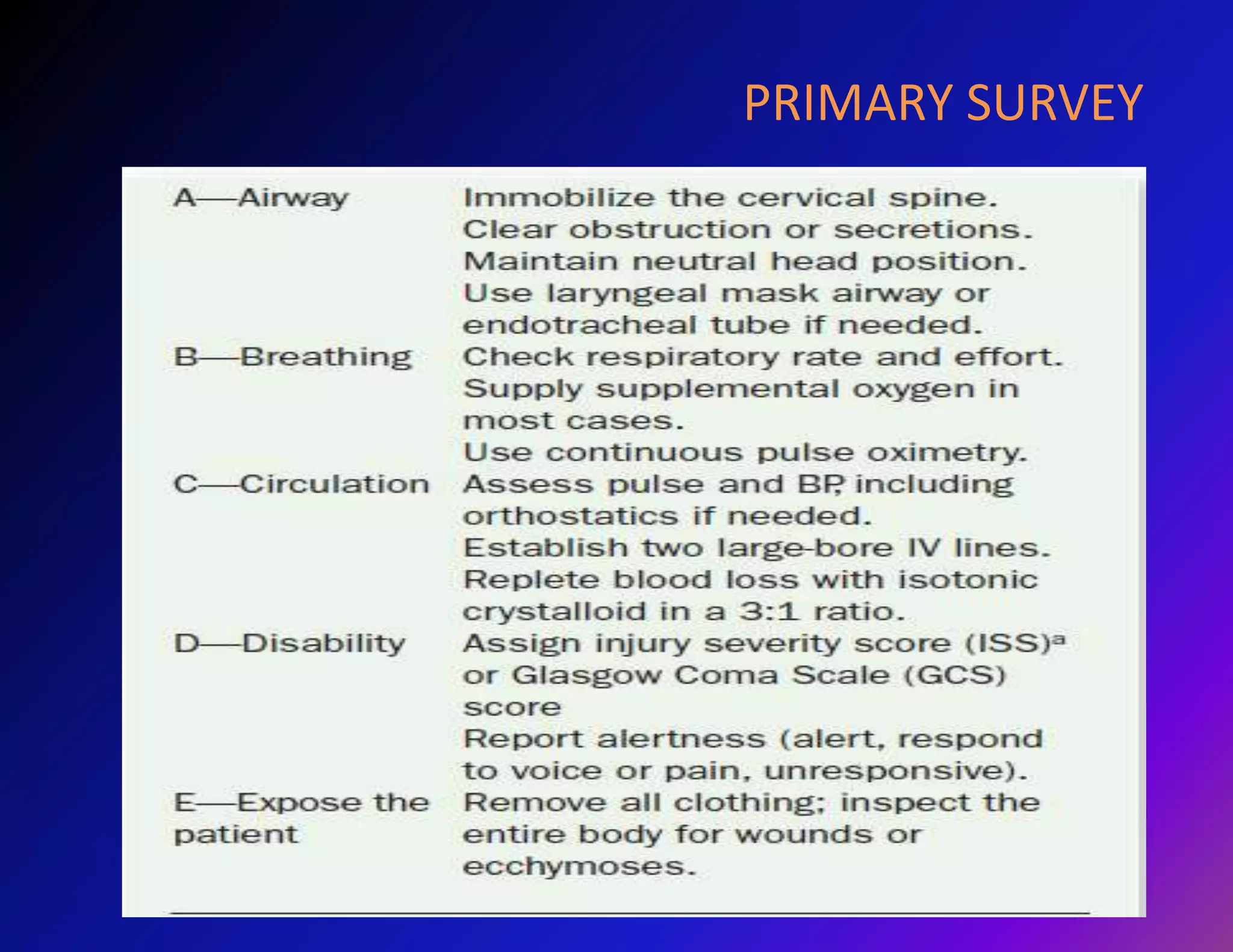
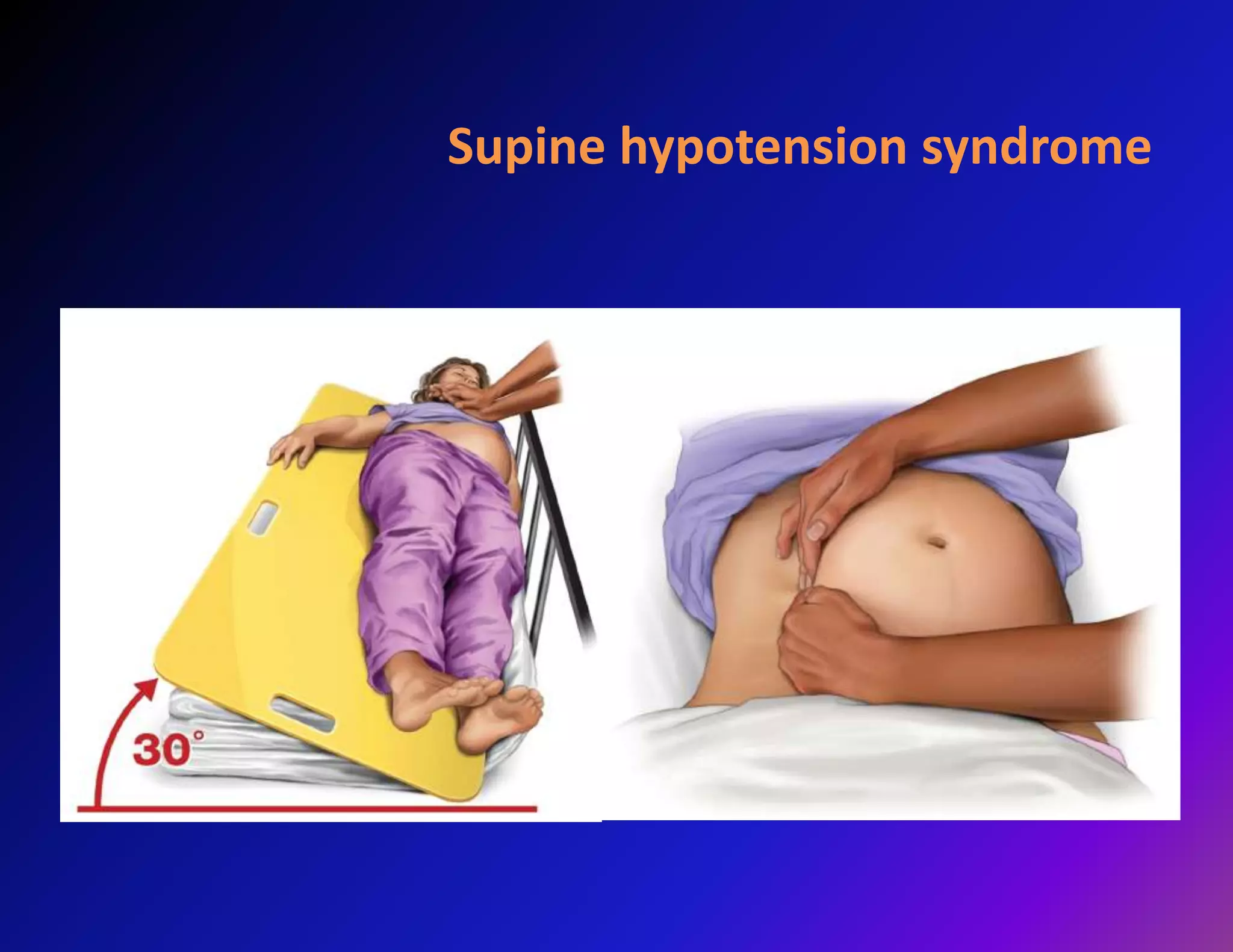
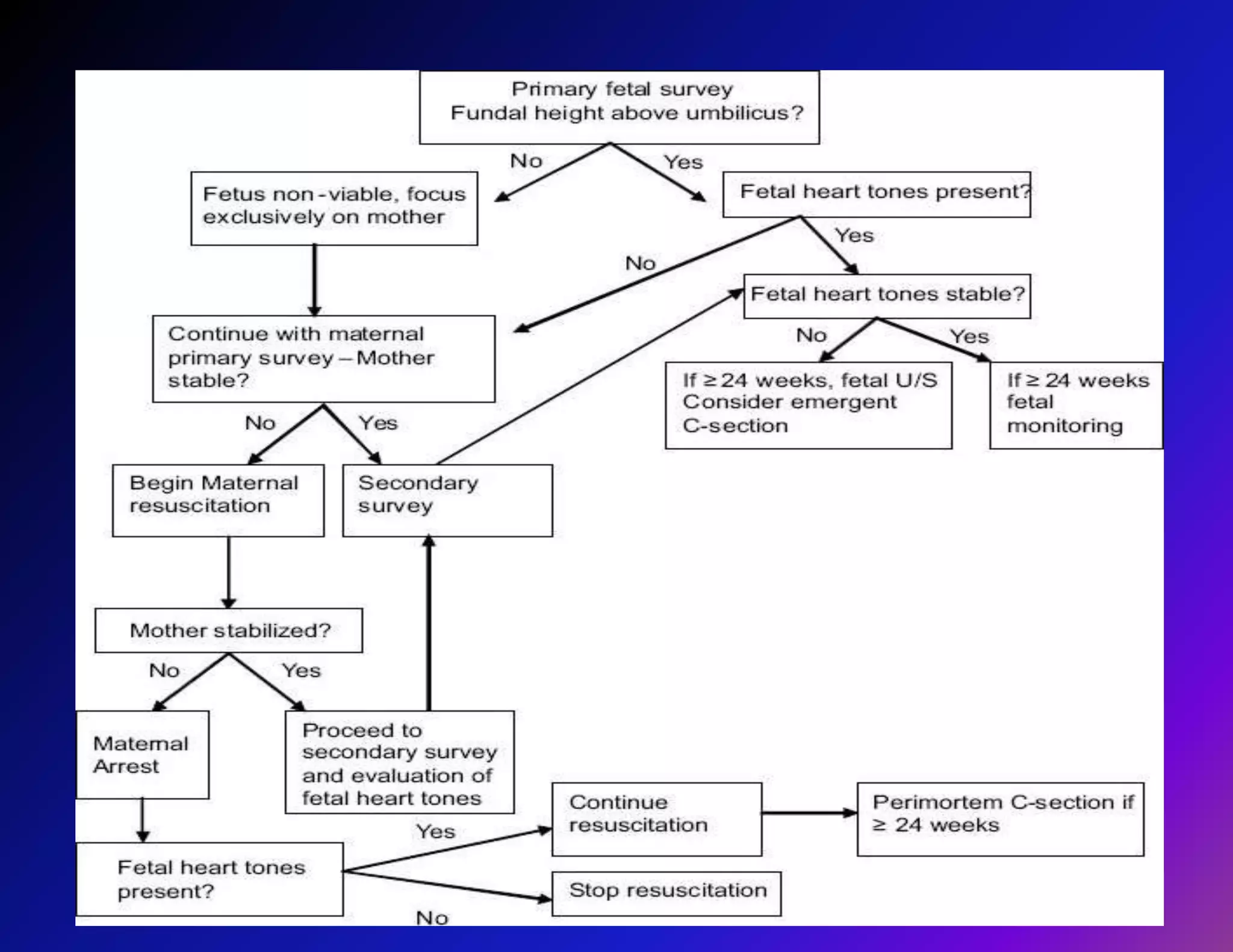
Trauma is a leading cause of non-obstetric death in pregnancy and can complicate 6-7% of pregnancies. The most common causes of trauma during pregnancy are motor vehicle collisions, assaults, falls, and domestic violence. Managing trauma in pregnancy requires a multidisciplinary approach and care of both the mother and fetus. The priorities are resuscitation of the mother to also resuscitate the fetus, assessment of fetal well-being, and treatment of maternal injuries while minimizing risks to the fetus. Diagnostic imaging such as ultrasound and CT scans can be used judiciously as long as radiation exposure is minimized. Timely delivery via c-section may be needed if the mother or fetus are critically unstable.