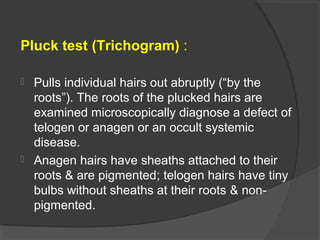
This document discusses various types and causes of hair loss. It begins by classifying hair loss as scarring vs nonscarring, and diffuse vs localized. Nonscarring hair loss can be caused by telogen effluvium (the most common cause), anagen effluvium, androgenetic alopecia, etc. Triggers of telogen effluvium include stress, medical conditions, nutritional deficiencies, and certain drugs. Evaluation involves history, examination including pull test and trichogram, and basic lab tests. Treatment focuses on identifying and removing triggers when possible as well as medications for specific conditions like minoxidil for androgenetic alopecia.