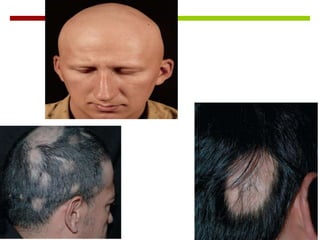
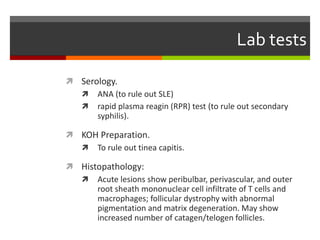
Alopecia areata is a non-scarring condition characterized by round or oval patches of hair loss with a generally good prognosis for limited cases. The etiology remains unknown but is associated with autoimmune diseases, and management options include intralesional steroids. Diagnosis may involve lab tests and histopathology, while psychological support and various therapies offer symptom relief but no cure.