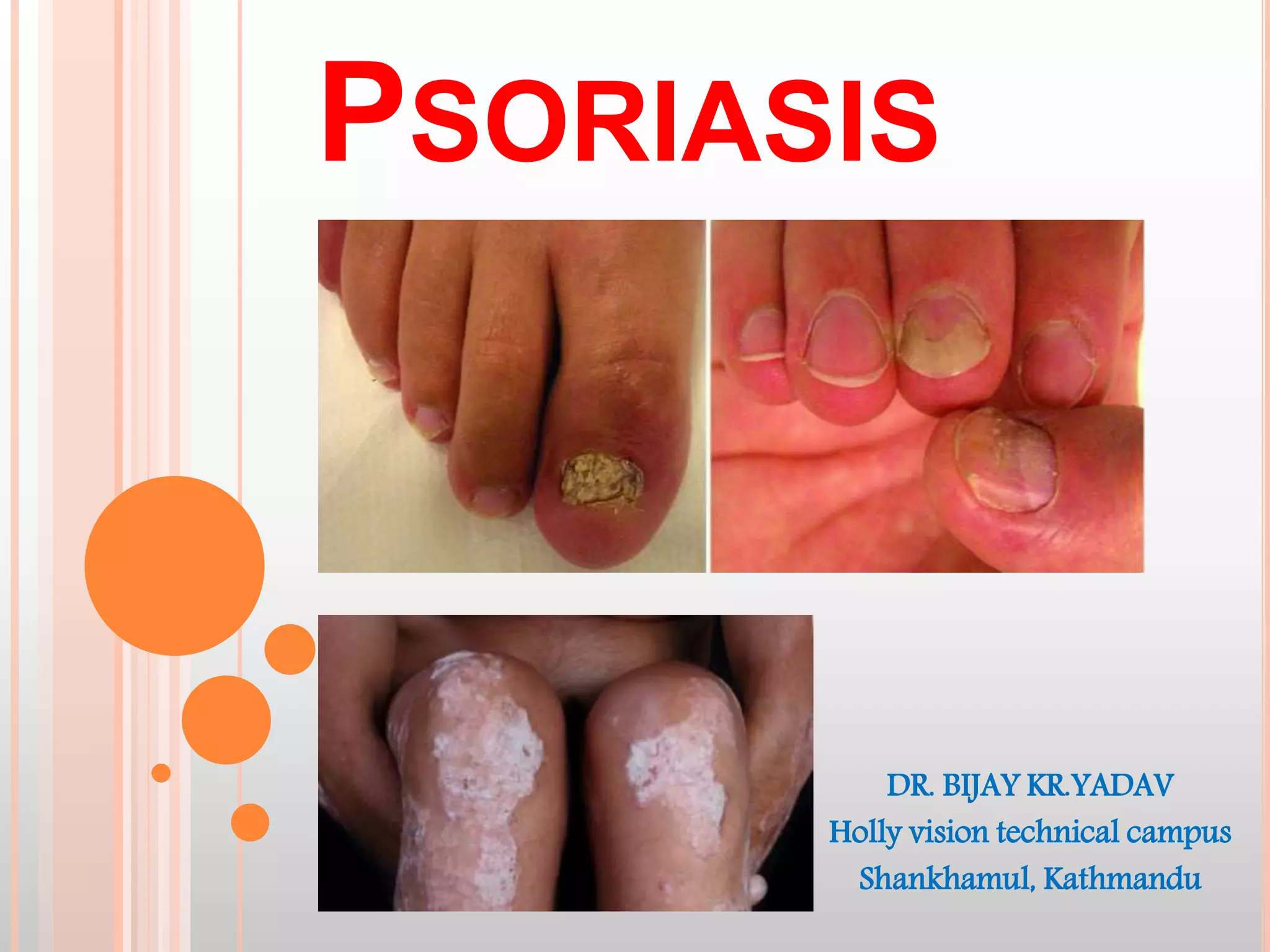
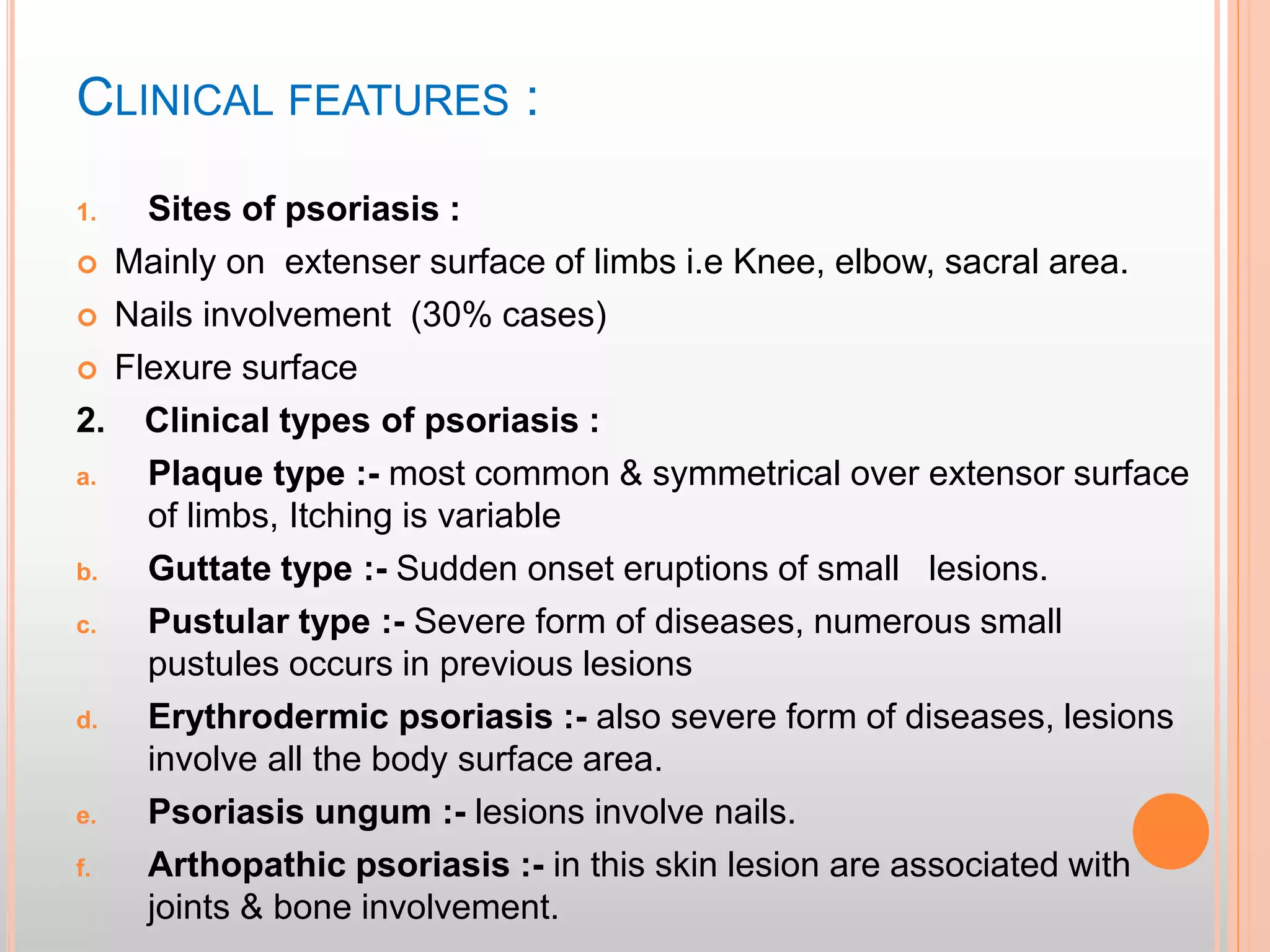
Psoriasis is a chronic, inflammatory skin condition characterized by red scaly patches that is genetically determined. It has various clinical types including plaque, guttate, pustular and erythrodermic psoriasis. Treatment involves topical therapies like emollients, dithranol and topical steroids. For moderate to severe cases, phototherapy using PUVA or systemic therapies like methotrexate are used. Management in health posts focuses initially on topical therapies with referral for extensive or pustular psoriasis requiring further treatment.