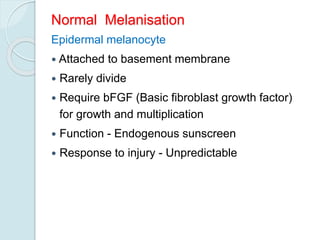
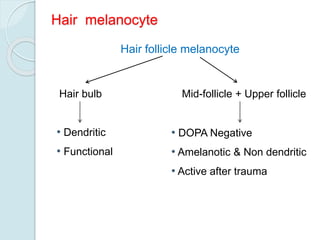
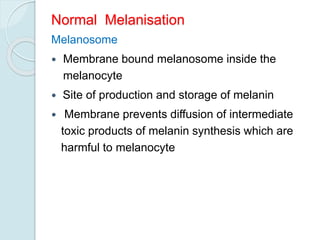
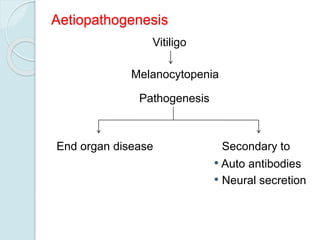
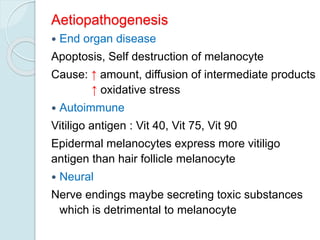
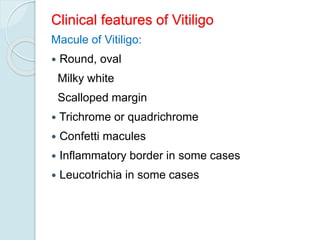
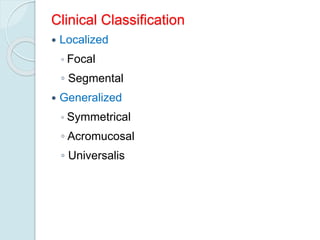
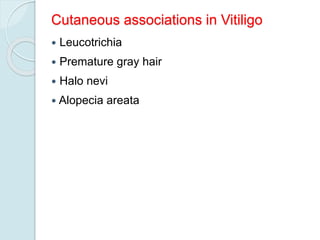
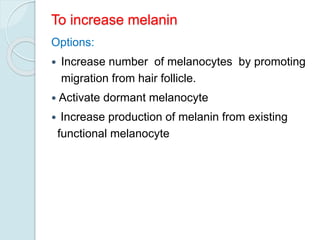
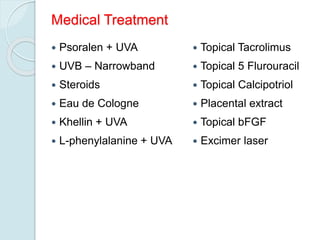
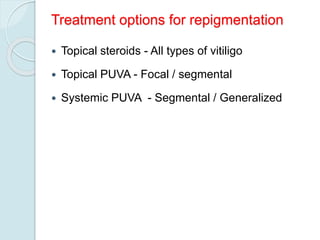
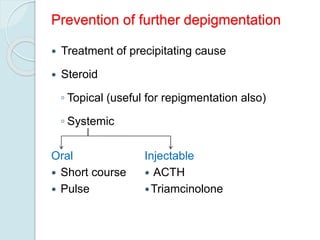
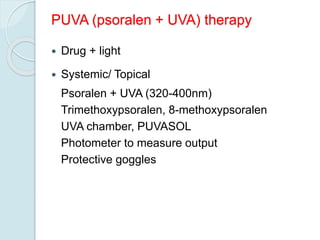
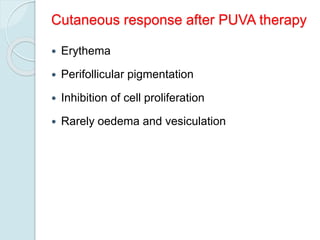
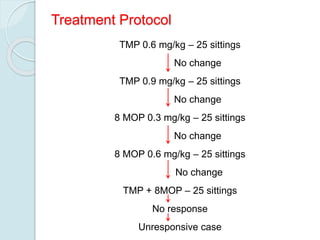
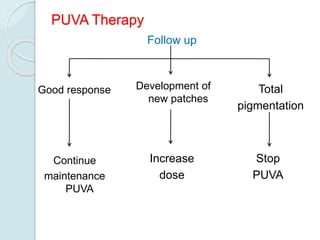
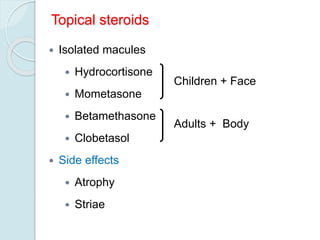
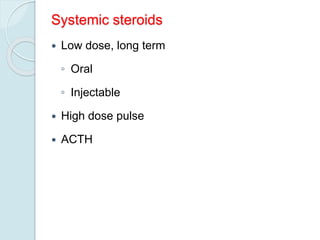
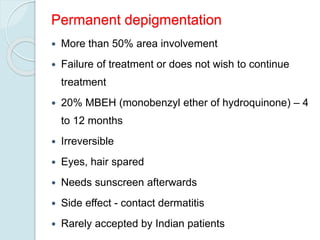
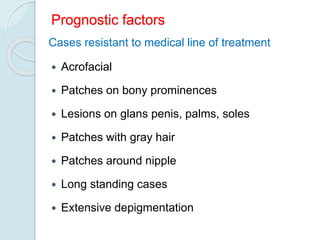
Vitiligo is a condition characterized by patches of skin that lose pigmentation due to the absence of melanocytes. It is caused by the destruction or malfunction of melanocytes, which may be due to autoimmune, neural, or endogenous factors. Treatment aims to repigment the skin and prevent further depigmentation, and involves topical agents like steroids and calcipotriol, phototherapy with UVB or PUVA, and surgical grafting in resistant cases. Vitiligo has no cure and treatment outcomes vary depending on the individual.