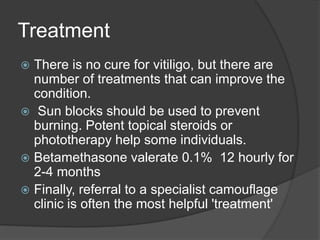
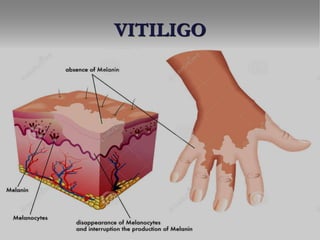
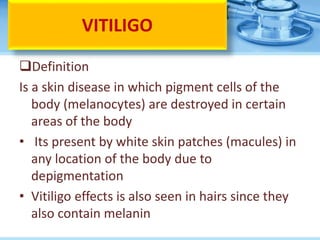
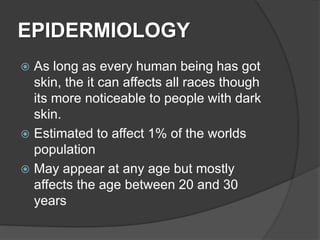
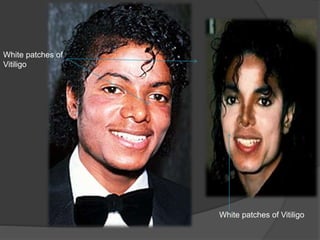
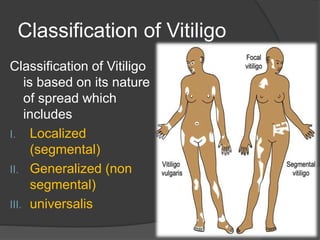
Vitiligo is a skin condition characterized by loss of pigment cells called melanocytes, resulting in white patches of skin. It affects around 1% of the world's population and can appear at any age, though most commonly between 20-30 years old. The cause is unknown but may involve an autoimmune response or oxidative stress damaging melanocytes. Vitiligo is classified based on distribution of the white patches and can be localized, generalized, or total body coverage. While there is no cure, treatments can help repigmentation and protection from sun damage is important to prevent complications.


![Investigations
Proper history taking and physical
examinations lead to diagnosis of Vitiligo.
Examine and rule out other medical
problems such as dermatitis or psoriasis.
Skin biopsy of the affected skin for cytology
Wood lamp examination
TSH levels [Thyroid disease].
• CBC [Pernicious anemia].
• Evaluation about Diabetes Mellitus.
• Ophthalmological examination](https://image.slidesharecdn.com/vitiligoreinty-190607101618/85/Vitiligo-presentation-21-320.jpg)