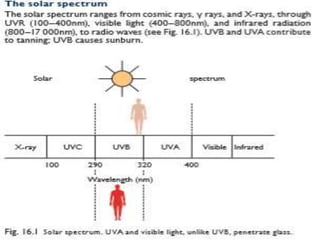
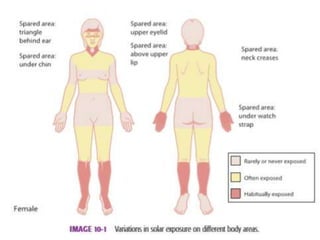
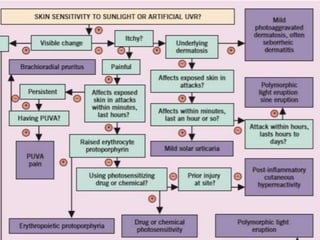
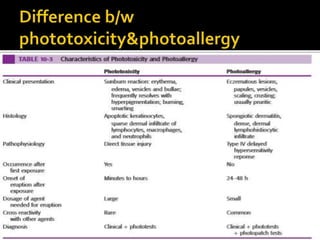
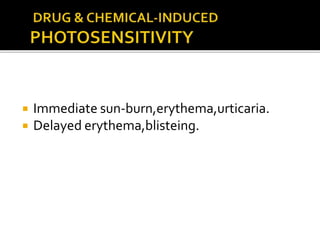
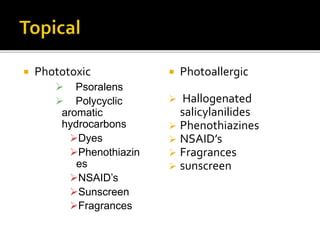
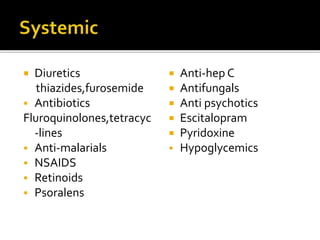
1. Cutaneous photosensitivity reactions require absorption of light energy by molecules, leading to damage and clinical disease.
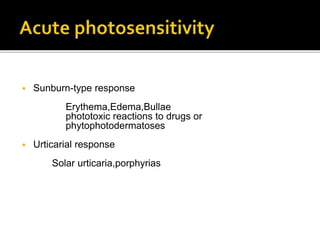
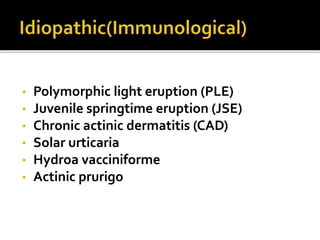
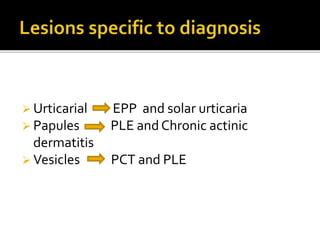
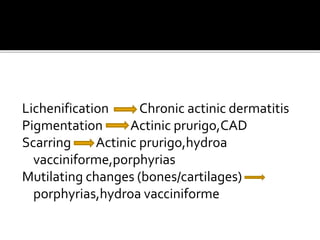
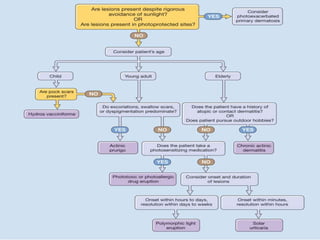
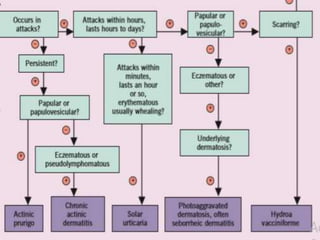
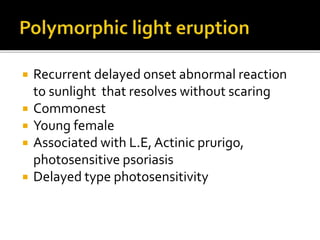
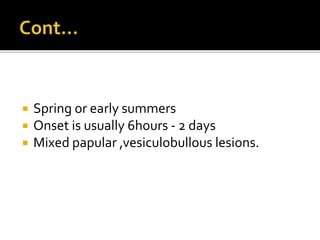
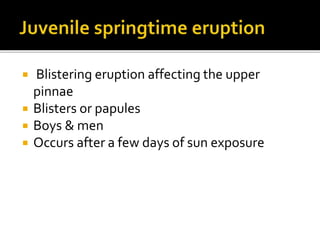
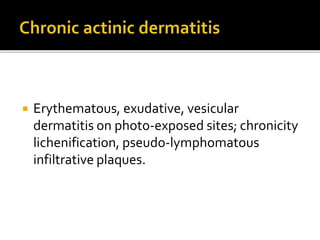
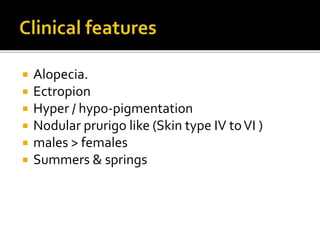
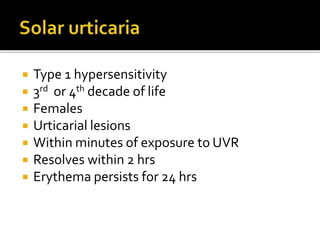
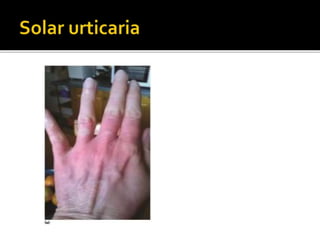
2. Common photosensitivity disorders include polymorphic light eruption (PLE), chronic actinic dermatitis (CAD), and solar urticaria.
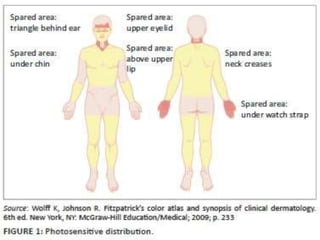
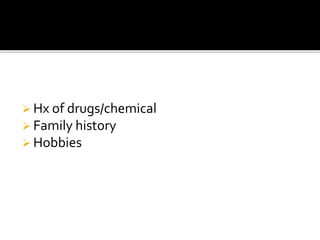
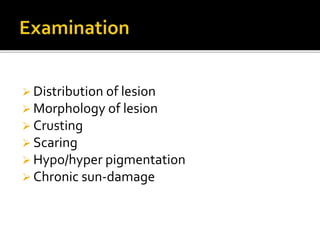
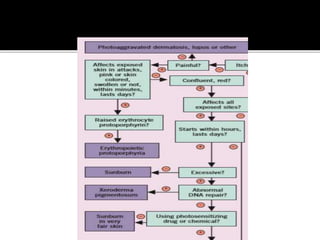
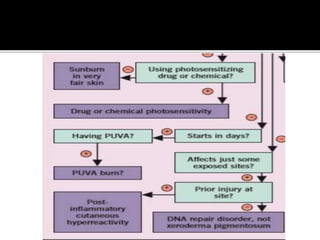
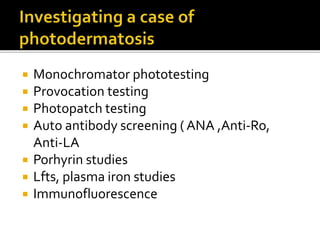
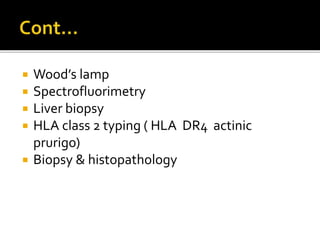
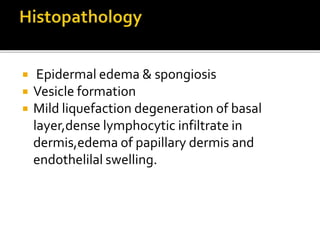
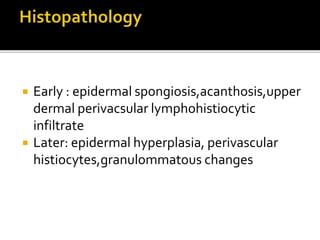
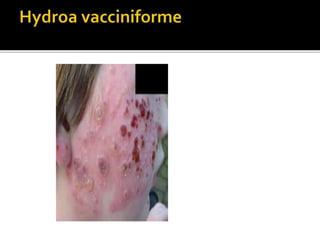
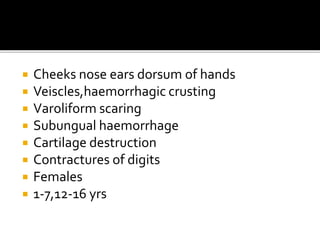
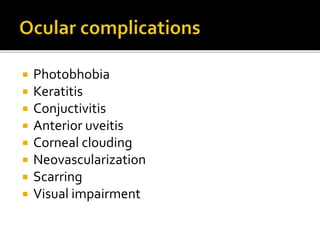
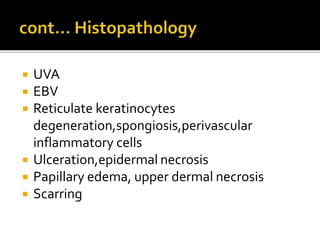
3. Clinical features, histopathology, and phototesting help differentiate types of photosensitivity dermatoses.