10. Leprosy
- 1. DR. BIJAY KR.YADAV Holly vision technical campus Shankhamul, Kathmandu
- 2. Leprosy ( Hansen’s disease) A chronic infectious disease caused by the bacterium “Mycobacterium Laprae” It is mainly a Granulomatous disease affecting : peripheral nerves & mucosa of the upper respiratory tract. “Gerhard Henrik Armauer Hansen” was a physician which 1st identified M. Leprae as the cause of leprosy in 1873 Mycobacterium leprae is gram-positive & belongs to: • kingdom: : Bacteria • Family : Mycobacteriaceae • Genus : Mycobacterium • Spacies : M. leprae
- 3. Epidemiological factors Occurs at all age groups Peak age of onset : Between 10 – 20 years Males > Females Children most susceptible Immune status ( host resistance) Overcrowding Low socioeconomic status
- 4. Transmission of Leprosy Respiratory route : Inhalation of bacilli-laden droplets Cutaneous : Skin to skin contact GIT : Ingestion of food Intradermal : Inoculation by tattoos } Not Yet Proven
- 6. Classification : A. Ridley & Jopling classification: Based on clinical, immunologic, histologic and bacteriologic finding. 1. Tuberculoid Leprosy (TT) 2. Borderline tuberculoid leprosy (BT) 3. Borderline Borderline leprosy (BB) 4. Borderline lepromatous leprosy (BL) 5. Lepromatous leprosy (LL)
- 7. B. Indian classification Non- lepromatous Indeterminate Lepromatous •Maculo- anesthetic •Tuberculoid •polyneuritic •Indeterminate •Borderline •lepromatous
- 8. C. Therapeutic Classification (WHO) Paucibacillary leprosy (PB) Single lesion Paucibacillary leprosy (SLPB) Multibacillary leprosy (MB)
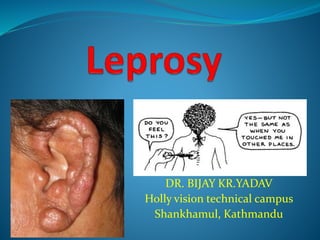
- 9. Clinical features : Cardinal signs : 1. Hypo pigmented / erythematous skin lesions with definite impairment of cutaneous sensations. 2. Enlargement and/ or tenderness of a peripheral nerves. 3. Skin smear for AFB Positive.
- 10. Indeterminate leprosy • Solitary • Ill-defined • Hypo pigmented macule • Only partially anesthetic
- 11. Tuberculoid (TT) Well defined Hypo pigmented lesion Dry surface Moderately raised margin. Completely anesthetic
- 12. Borderline Tuberculoid (BT) Erythemato- hypochromic plaque Dry surface Raised Well defined margins with satellite lesions Anesthetic
- 13. Borderline Borderline (BB) Erythematous Raised annular plaques with central clearing and sloping edges ( inverted saucer appearance ) Hypoesthetic Multiple, asymmetrically thickened nerves
- 14. Borderline Lepromatous (BL) Thick erythematous plaques on face and ears. Not sharply delimited. No sensory impairment.
- 15. Lepromatous Leprosy (LL) Extensive, symmetrically distributed infiltration almost coalescent macules and plaques. Not anesthetic.
- 16. General aspect of R-J classification Observation TT BT BB BL LL No. of lesions Single usually Single or few Several Many Very many Size of lesions Variable Variable Variable Variable Small Surface of lesions Very dry Dry Slightly shiny Shiny Shiny Sensation in lesion ( Not face) Absent Mod - markedly diminished Mod diminished Slightly diminished Not affected Hair growth in lesions Nil Markedly diminished Moderately diminished Slightly diminished Not affected AFB in lesions Nil Nil or scanty Moderate numbers Many Very many (globi) Lepromin test + + + + + or + + Negative Negative Negative
- 17. Diagnostic Tests Skin smears Nasal smears and nasal blows Skin biopsy Nerve biopsy Histamine test Sweating test Phenolic glycolipid (PGL-1) Polymerase chain reaction (PCR)
- 18. How to diagnose leprosy? Examine skin Check for patches Test for sensation Count the no. of patches Look for damage to nerves
- 19. Treatment of Leprosy In 1982 WHO recommended multi-drug therapy (MDT) Advantages of MDT: Better cure of the disease. Shortened duration of treatment. Better compliance by the patient. Less chance of drug resistant.
- 20. Paucibacillary Leprosy Skin lesions – Not more than 5. Nerves - Not more than 1. Skin smear – Negative. Treatment : PB leprosy (TT and BT) Monthly supervised: Rifampicin 600mg Daily, unsupervised: Dapsone 100mg. Duration of treatment - 6 months.
- 21. In Single lesion Paucibacillary leprosy (SLPB): Only one anesthetic skin lesion and no nerve involvement & AFB is –ve Single dose ROM Therapy: (R) Rifampicin 600mg (O) Ofloxacin 400mg (M) Minocycline 100mg
- 22. Multibacillary Leprosy Skin Lesions - More than 5. Nerve - More then 1. Skin smear for AFB - Positive. Treatment : Monthly, supervised : Rifampicin 600mg, Clofazamine 300mg Daily, unsupervised: Dapsone 100mg, Clofazamine 50mg. Duration of treatment: 1 year.
- 23. Leprosy reaction ( Reactional States ) A. Type 1 lepra reaction B. Type 2 lepra reaction
- 24. Type 1 lepra Reaction Type 1 lepra reaction is due to sudden improvement of Cell mediated immunity CMI (Upgrading or Reversal) or worsening of CMI (Downgrading). Skin lesions - Erythema, swelling, tenderness of some or all lesions, shiny, warm to touch. Fever and malaise: Unusual Nerve - swollen, tender and painful. (sometimes nerve abscesses).
- 25. Treatment Prompt treatment is of vital importance as permanent nerve damage can occur. Oral Prednisone in tapering doses. Symptomatic treatment. Rest and splint.
- 26. Type 2 reaction Also known as Erythema nodosum leprosum mediated through humoral immunity. Occurs in lepromatous and few cases of BL. Reaction due deposition of antigen antibody complexes in the lesions. C/F: ENL, neuritis, bone pain, joint pain, fever, malaise, lymphadenitis, rhinitis, epistaxis, iritis, epididymo- orchitis, proteinuria.
- 27. Treatment Thalidomide NSAIDs Clofazimine Corticosteroids (Prednisolone).
