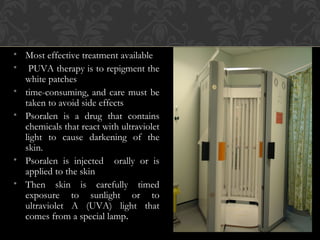
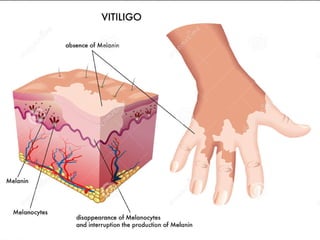
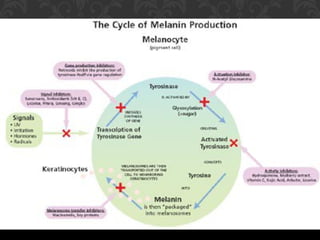
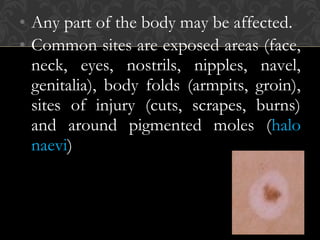
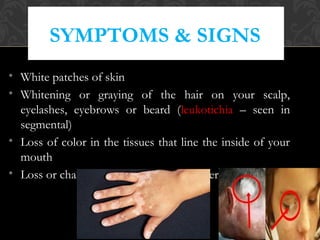
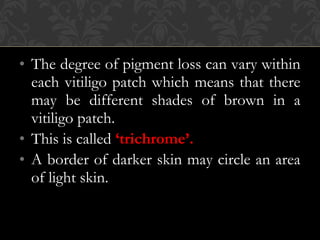
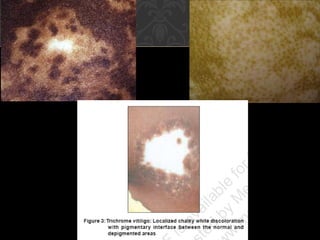
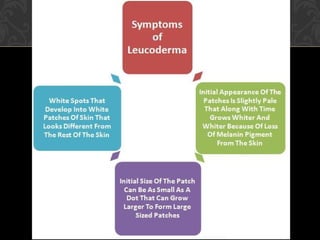
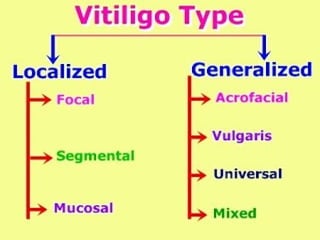
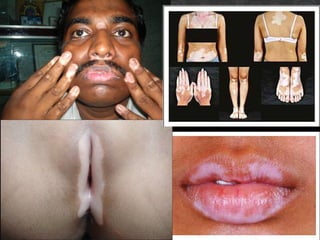
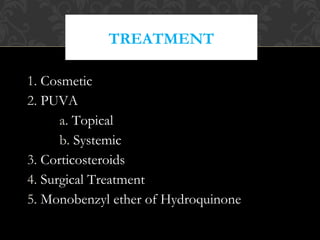
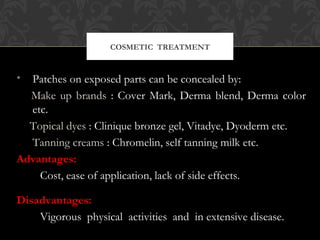
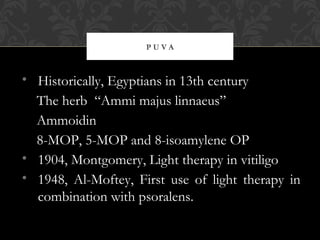
Melanin is the pigment produced by melanocytes in the skin that determines skin color. It protects the skin from UV damage. Vitiligo is a condition where melanocytes die or stop functioning, causing white patches of skin where no melanin is produced. It can affect any part of the body and is associated with autoimmune diseases. Treatments include cosmetic camouflage, phototherapy (PUVA), topical corticosteroids, and skin grafting. Prognosis varies and vitiligo may continue in cycles of pigment loss and stability.
![SYSTEMIC
ASSOCIATIONS
• ↑ risk of Autoimmune diseases.
• Thyroid dis. [Hashimoto’s, Grave’s]
• Addison’s disease
• Pernicious Anemia
• Insulin dependent Diabetes
• Alopecia Areata](https://image.slidesharecdn.com/vitiligo-140730081232-phpapp02/85/Vitiligo-22-320.jpg)
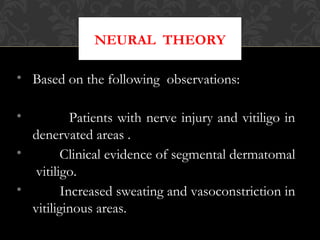
![NEURAL THEORY…
[CONT.]
• Depigmentation in animal models with severed
nerve fibres.
• Degenerative and regenerative autonomic
nerves in depigmented patches.
• Increased urinary excretion of VMA and HVA
in active vitiligo.](https://image.slidesharecdn.com/vitiligo-140730081232-phpapp02/85/Vitiligo-31-320.jpg)
![EVALUATION
• Total body Wood’s light examination.
• TSH levels [Thyroid disease].
• CBC [Pernicious anemia].
• Evaluation about Diabetes Mellitus.
• Ophthalmological examination.](https://image.slidesharecdn.com/vitiligo-140730081232-phpapp02/85/Vitiligo-37-320.jpg)
![MECHANISM OF ACTION [PUVA]
• Immunologically mediated action.
• Stimulation of tyrosinase activity.
• Inhibition of DNA and protein synthesis.
• Depletion of EGF expression.
• Depletion of vitiligo - associated melanocyte
antigens.](https://image.slidesharecdn.com/vitiligo-140730081232-phpapp02/85/Vitiligo-41-320.jpg)
![MELANOCYTE
REPIGMENTATION
• Activation of inactive cells [spared in vitiligo
process] in the middle and lower part of follicle
and in outer sheath.
• These inactive cells contain structural and
melanosomal proteins, but do not contain
enzymes, required for melanogenesis.](https://image.slidesharecdn.com/vitiligo-140730081232-phpapp02/85/Vitiligo-42-320.jpg)
![MELANOCYTE REPIGM. [CONT.]
• Migration of melanocyte from lower hair follicle to
epidermis, depends on :
a) Cytokine release, like FGF, IL-1,
b) Inflammatory mediators such as : TGF-α,
leukotriene C4, D4, and endothelin-1.](https://image.slidesharecdn.com/vitiligo-140730081232-phpapp02/85/Vitiligo-43-320.jpg)