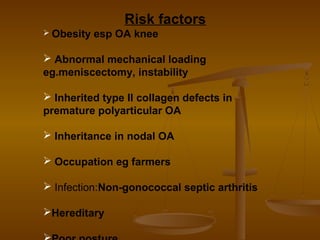
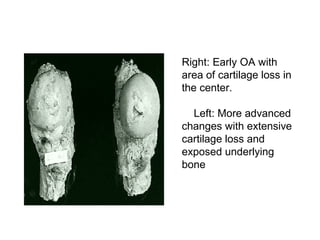
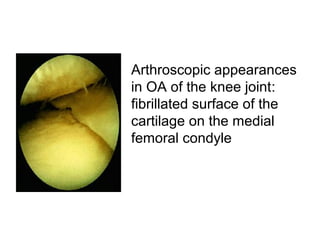
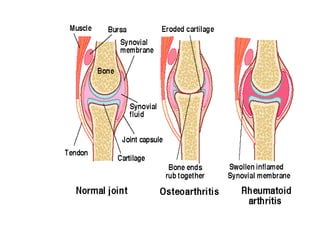
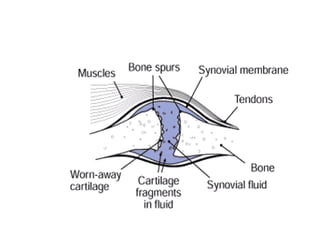
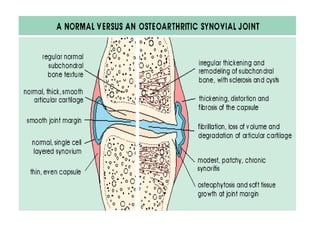
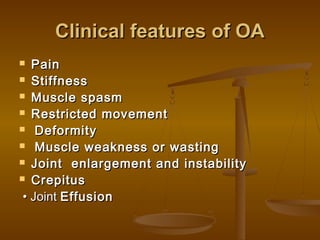
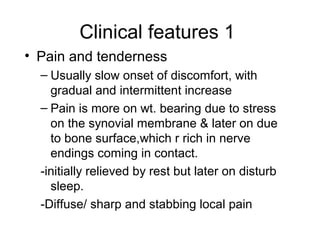
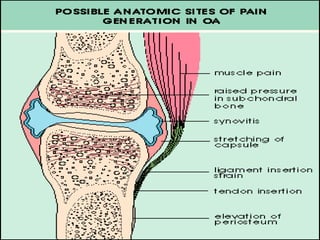
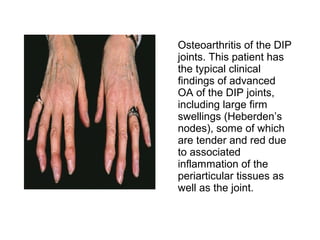
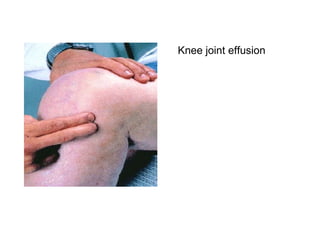
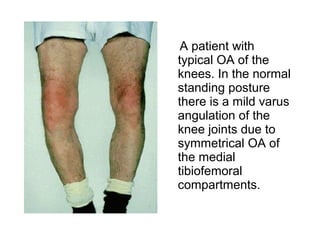
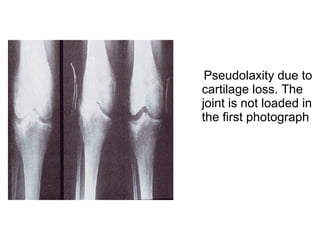
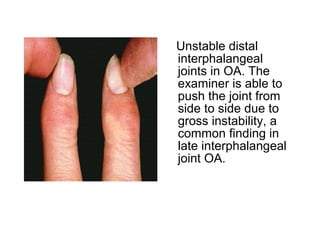
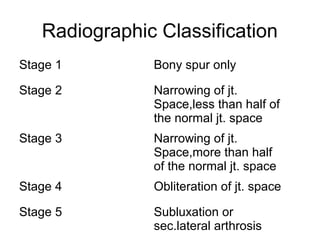
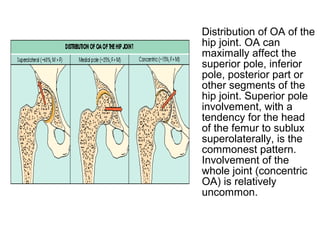
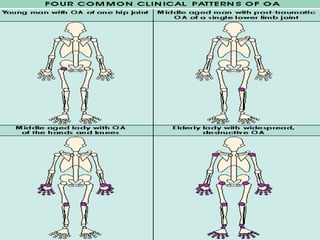
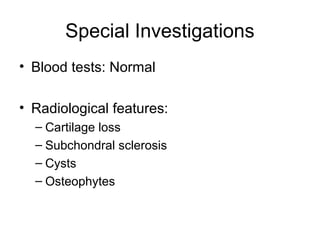
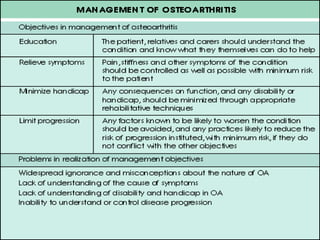
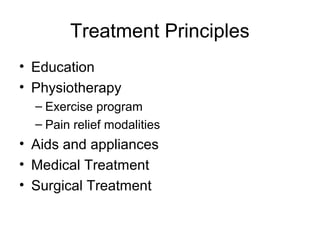
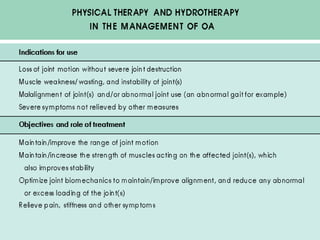
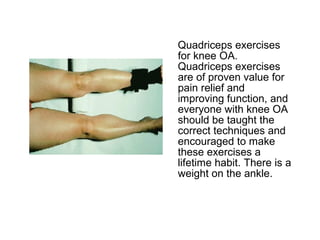
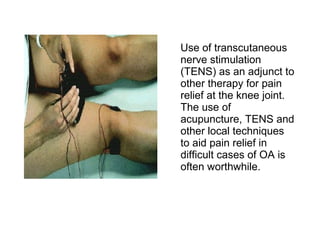
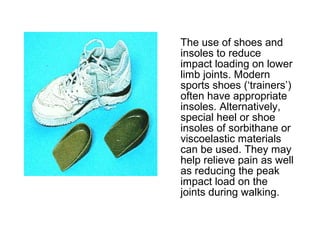
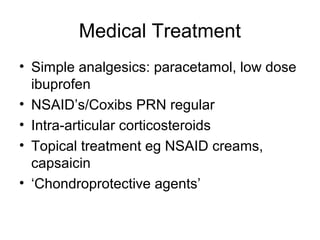
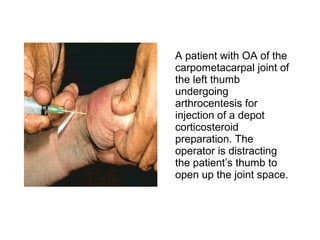
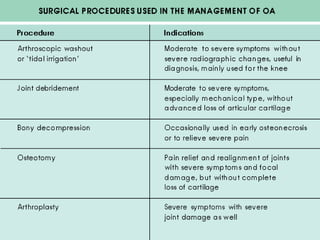
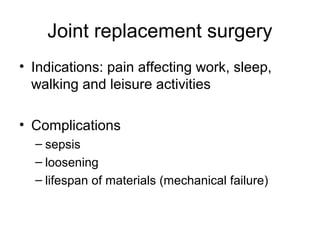
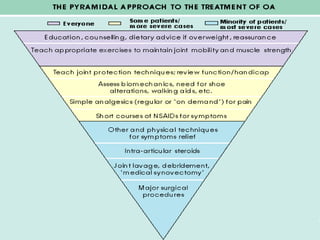
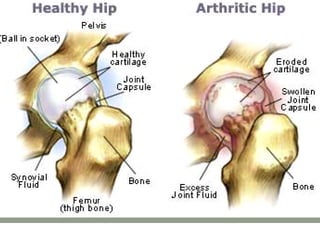
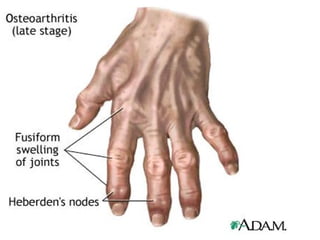
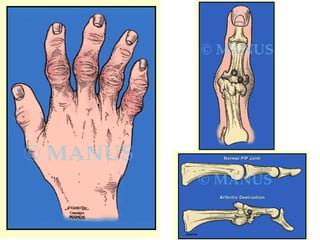
Osteoarthritis is a degenerative joint disease characterized by breakdown of cartilage and bone changes. It most commonly affects weight-bearing joints like the hips and knees. Risk factors include obesity, joint injury, genetics, and age. Symptoms include joint pain, stiffness, swelling, and decreased range of motion. Diagnosis is made based on clinical features and confirmed with x-rays showing cartilage loss, bone spurs, and bone changes. Treatment focuses on education, exercises, braces, medications, and sometimes surgery to relieve symptoms and improve function.