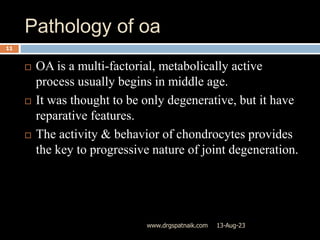
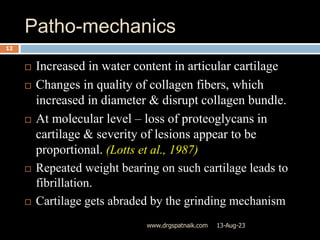
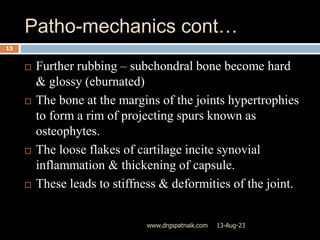
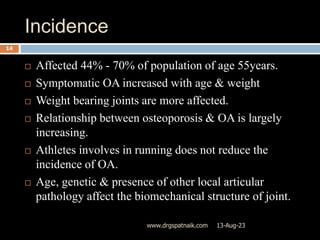
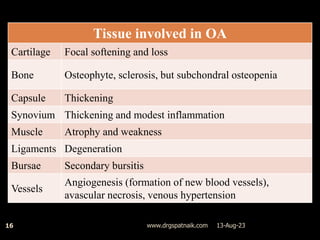
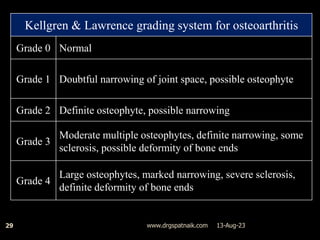
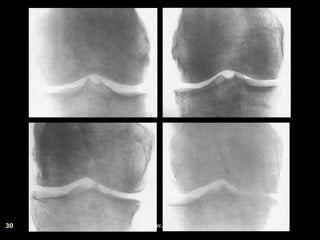
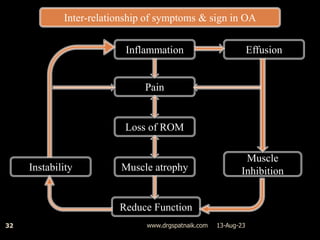
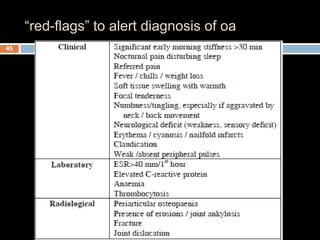
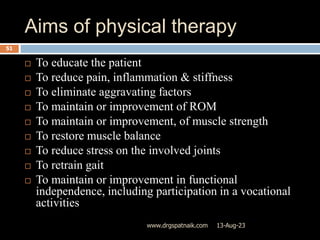
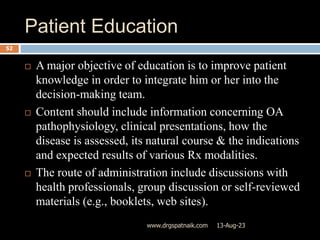
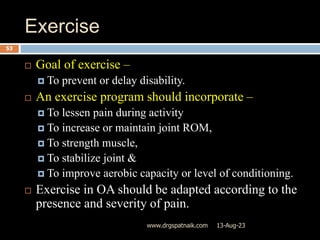
Osteoarthritis (OA) is a common degenerative joint disease affecting synovial joints. It involves breakdown of cartilage and underlying bone. Key features include joint pain, stiffness, and loss of function. Risk factors include older age, obesity, joint injury, and genetic predisposition. Diagnosis is based on clinical history, physical exam, and x-ray findings such as joint space narrowing and osteophyte formation. Physical therapy aims to reduce pain and improve function through exercises and other conservative treatments.