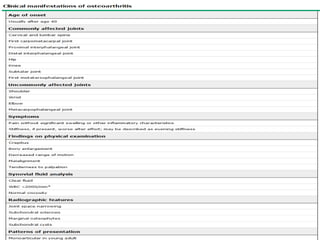
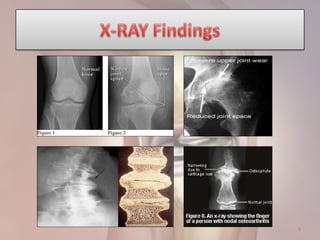
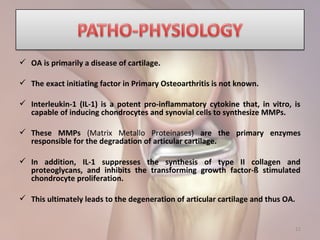
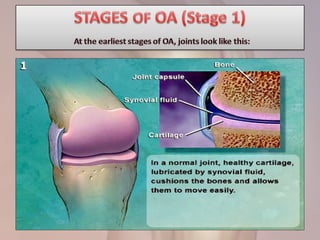
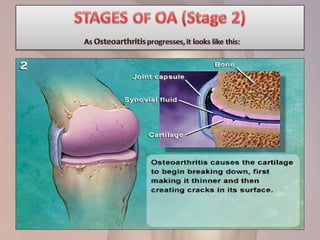
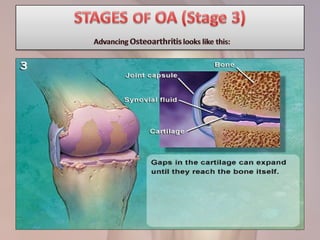
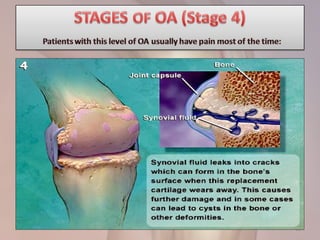
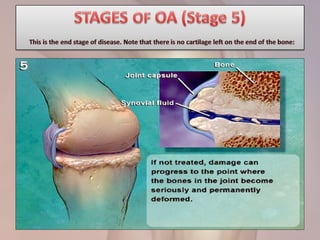
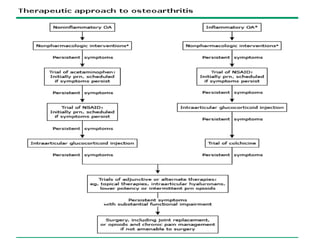
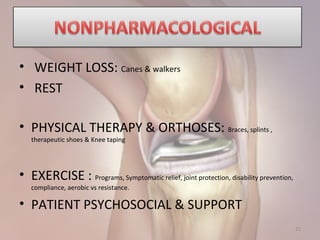
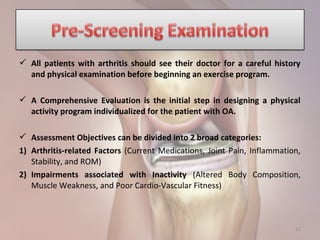
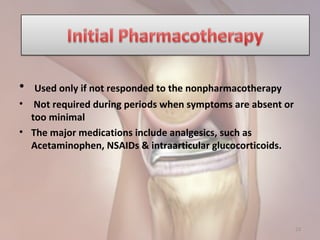
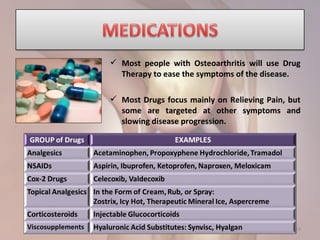
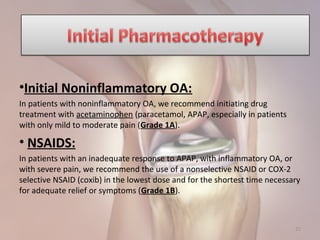
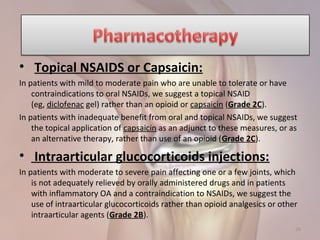
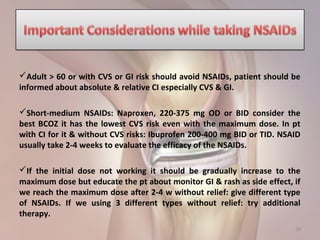
Osteoarthritis is a chronic condition characterized by the breakdown of cartilage in a joint, causing bones to rub together and leading to pain, stiffness, and loss of movement. It is most commonly caused by aging but can result from other factors like injury or genetics. Symptoms usually appear in middle age and worsen with age. Treatment focuses on reducing pain and inflammation, improving mobility, and preventing further joint damage through weight loss, physical therapy, braces, and medications like acetaminophen, NSAIDs, or corticosteroid injections. For those not helped by initial treatments, options include topical agents, opioids, viscosupplementation, or surgery. The goals of treatment are to control symptoms and preserve function.