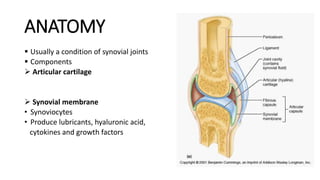
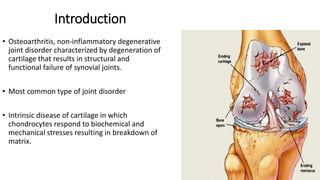
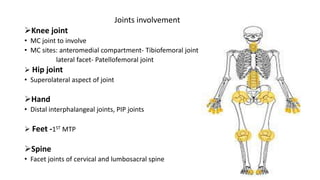
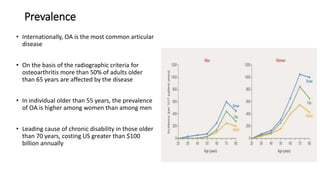
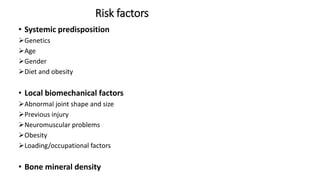
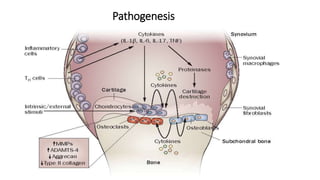
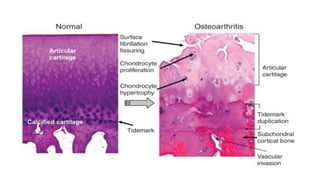
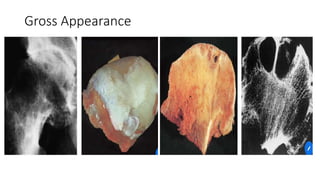
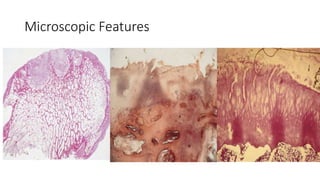
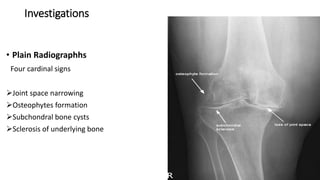
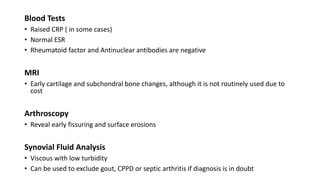
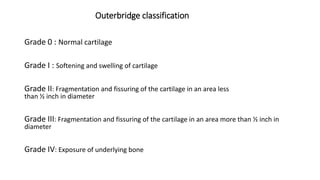
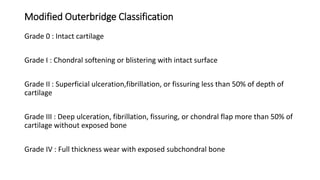
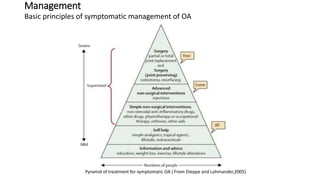
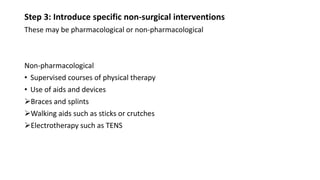
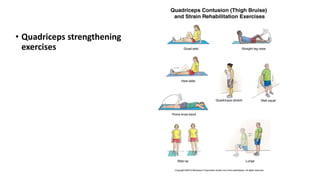
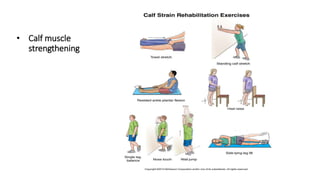
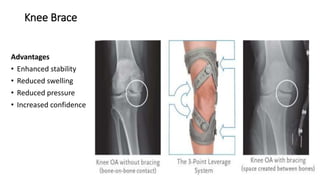
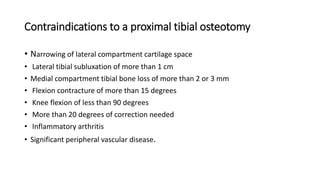
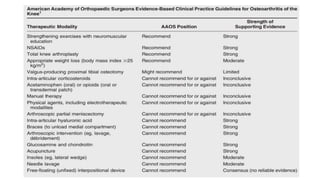
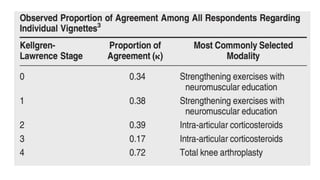
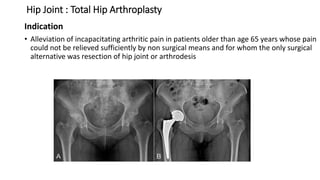
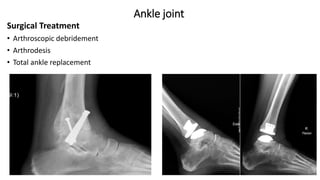
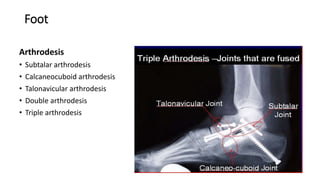
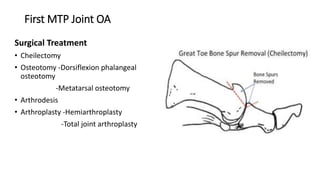
Osteoarthritis is a degenerative joint disease characterized by breakdown of cartilage. It most commonly affects weight-bearing joints like the knee, hip, and hand. Risk factors include age, obesity, previous injury, and genetics. Symptoms include pain, stiffness, swelling, and decreased range of motion. Diagnosis is based on x-rays showing joint space narrowing, osteophytes, and bone changes. Treatment focuses on reducing pain and inflammation with medications and physical therapy. For advanced disease, options include joint injections, bracing, and surgery like arthroscopy, joint replacement, or fusion.