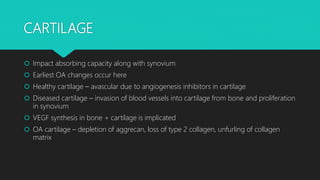
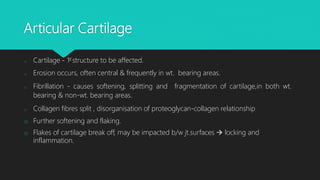
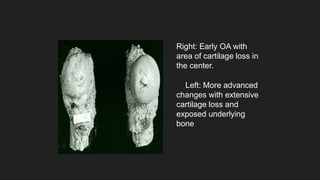
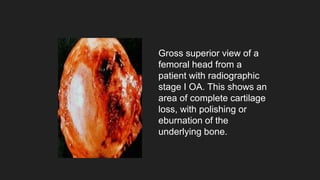
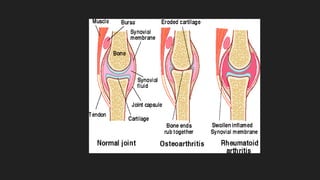
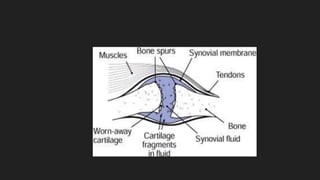
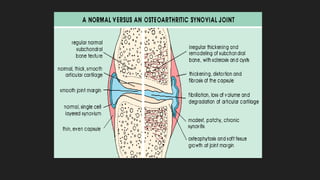
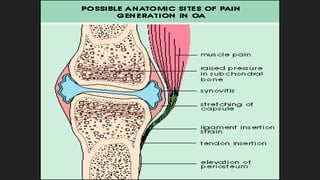
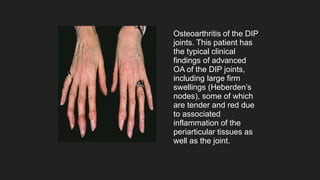
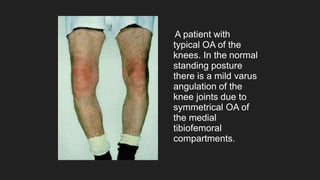
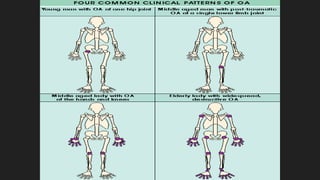
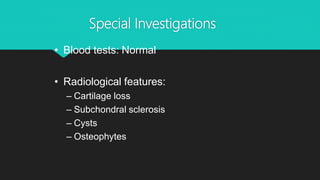
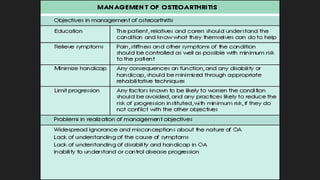
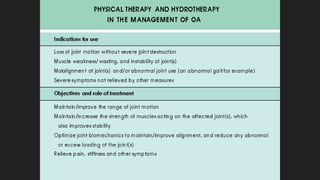
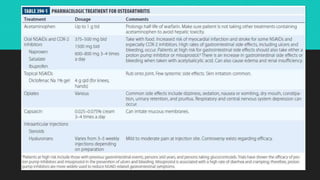
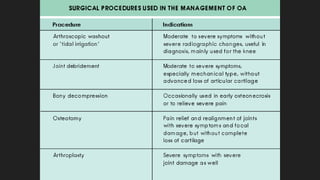
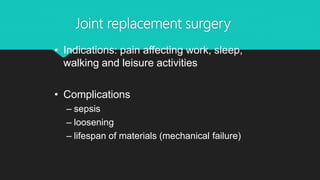
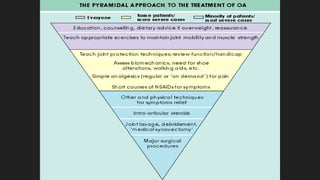
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage. It most commonly affects weight-bearing joints like the hips and knees. The cartilage, bone, synovial membrane, capsule, ligaments and muscles are all affected as the disease progresses. Symptoms include joint pain and stiffness that worsens with use of the affected joint. Treatment focuses on reducing pain and inflammation, maintaining joint mobility, and may include joint replacement surgery for severe cases.