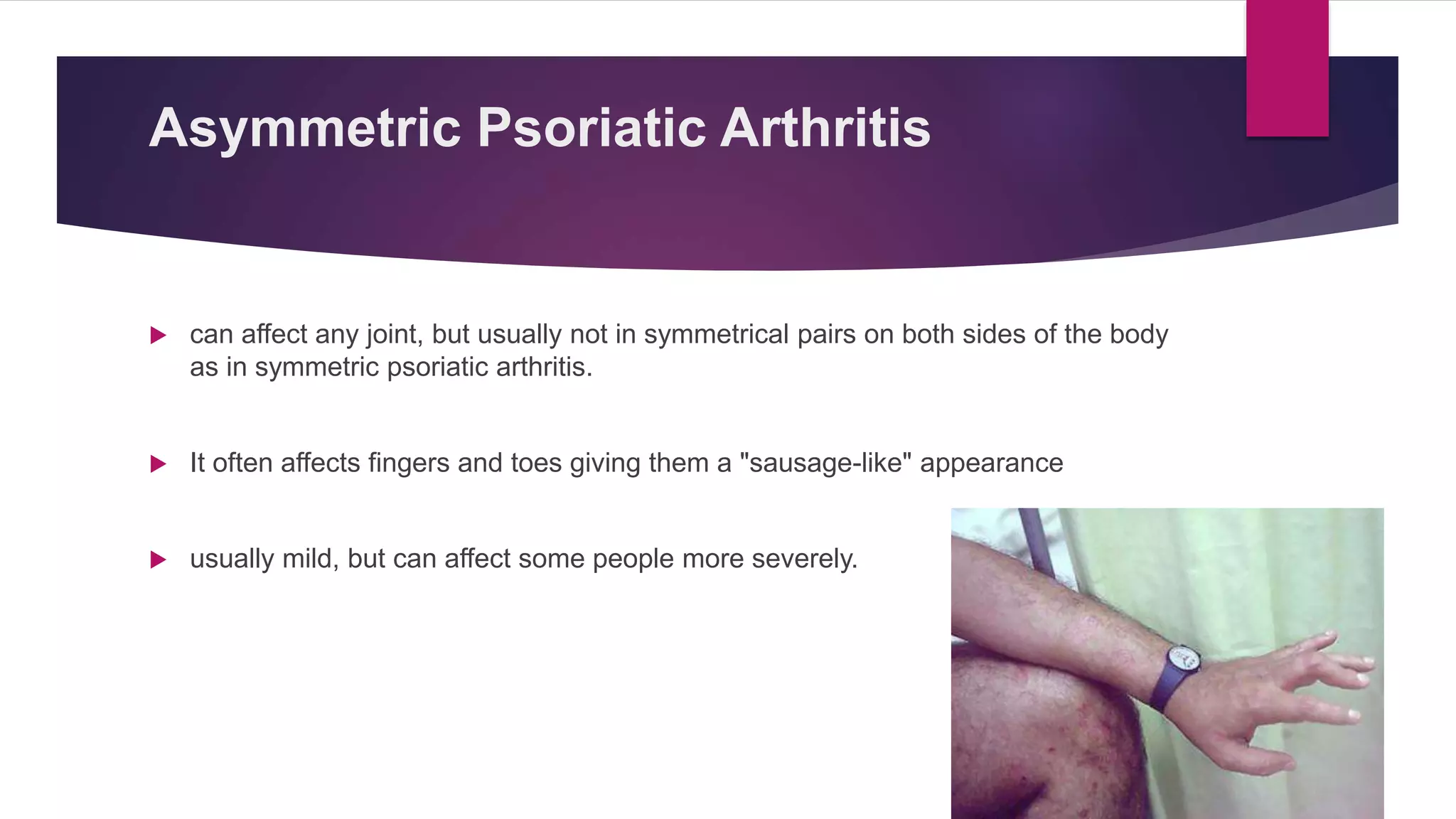
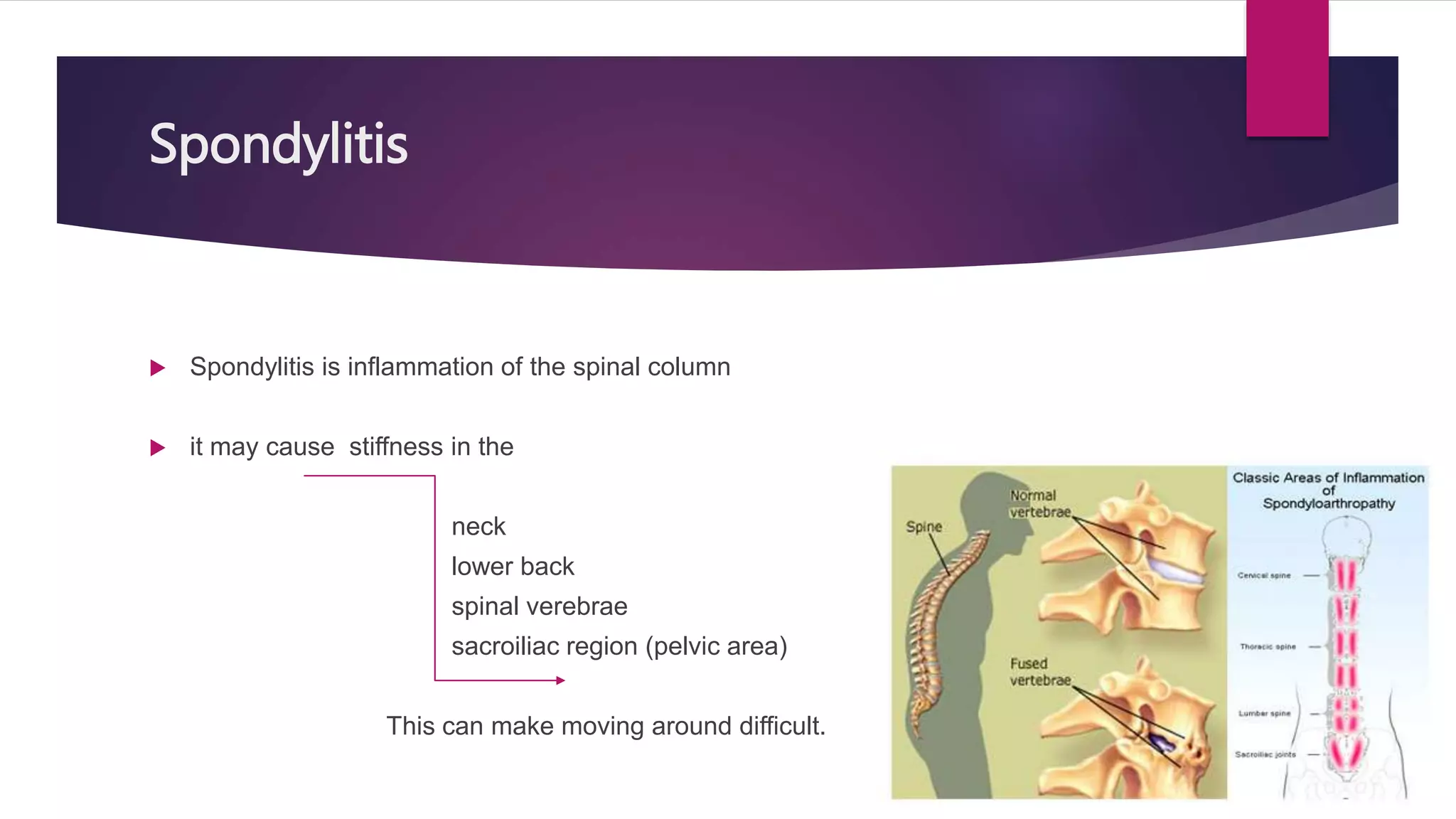
Psoriatic arthritis is a chronic inflammatory disease characterized by psoriasis of the skin and arthritis of the joints. It affects 15-25% of people with psoriasis. The causes are unknown but involve genetic and immune factors. Risk factors include family history of psoriasis. Symptoms include swollen, painful, stiff joints, especially in the knees, ankles, fingers and toes. There are five types classified by the joints affected and severity. Treatment involves medications like NSAIDs, methotrexate, exercise and assistive devices, with the goal of managing symptoms and slowing progression as there is no cure currently.