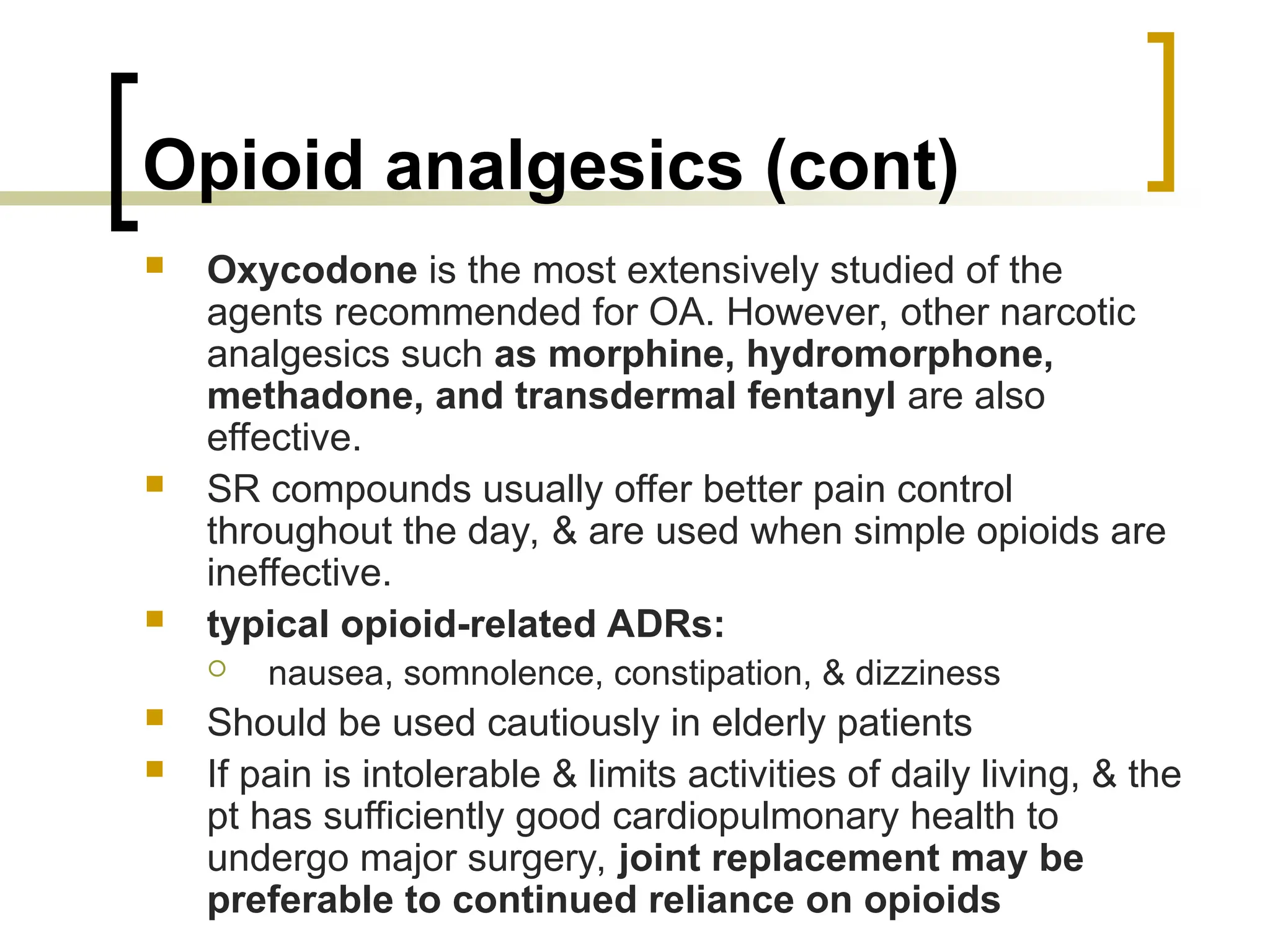
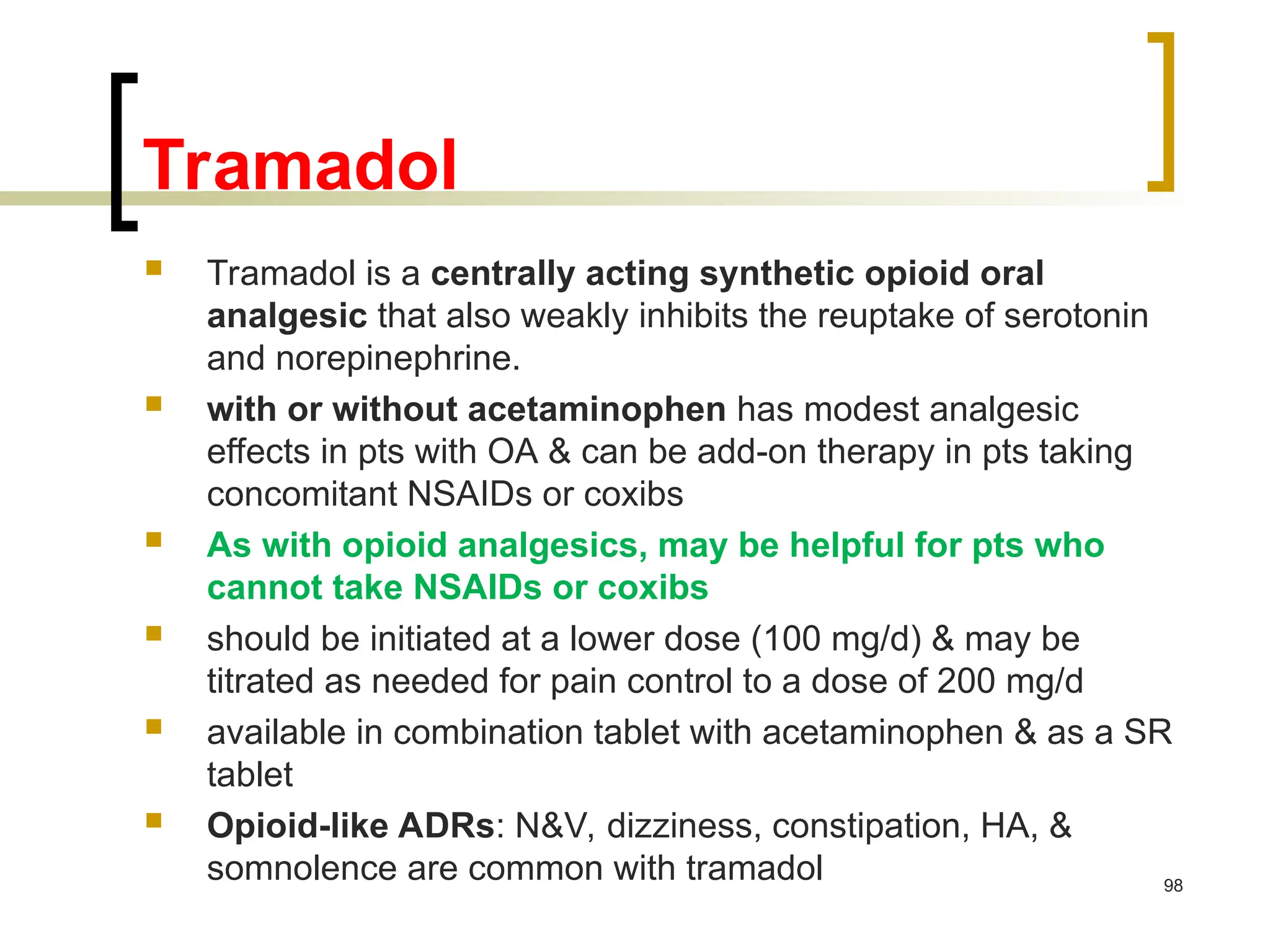
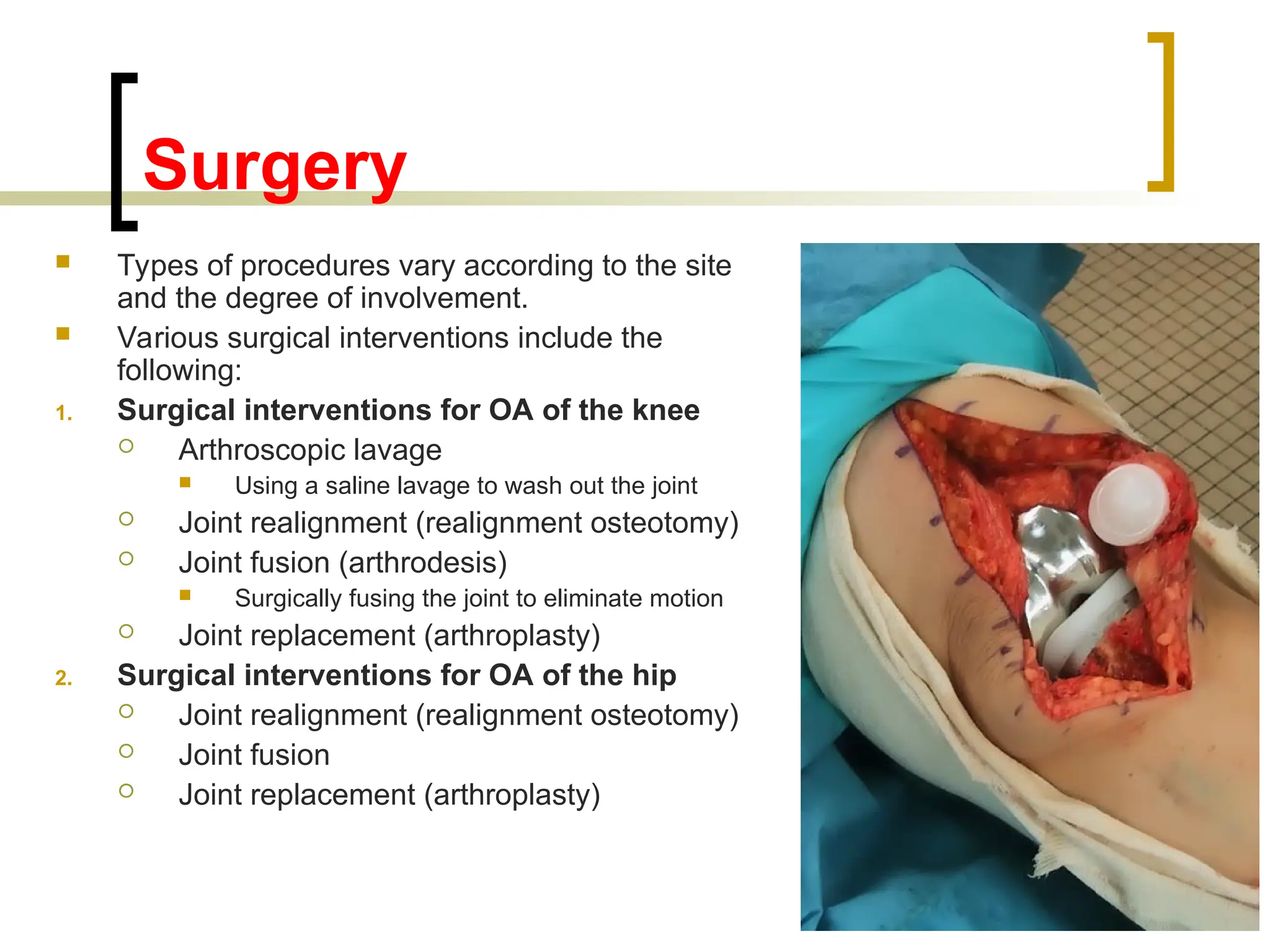
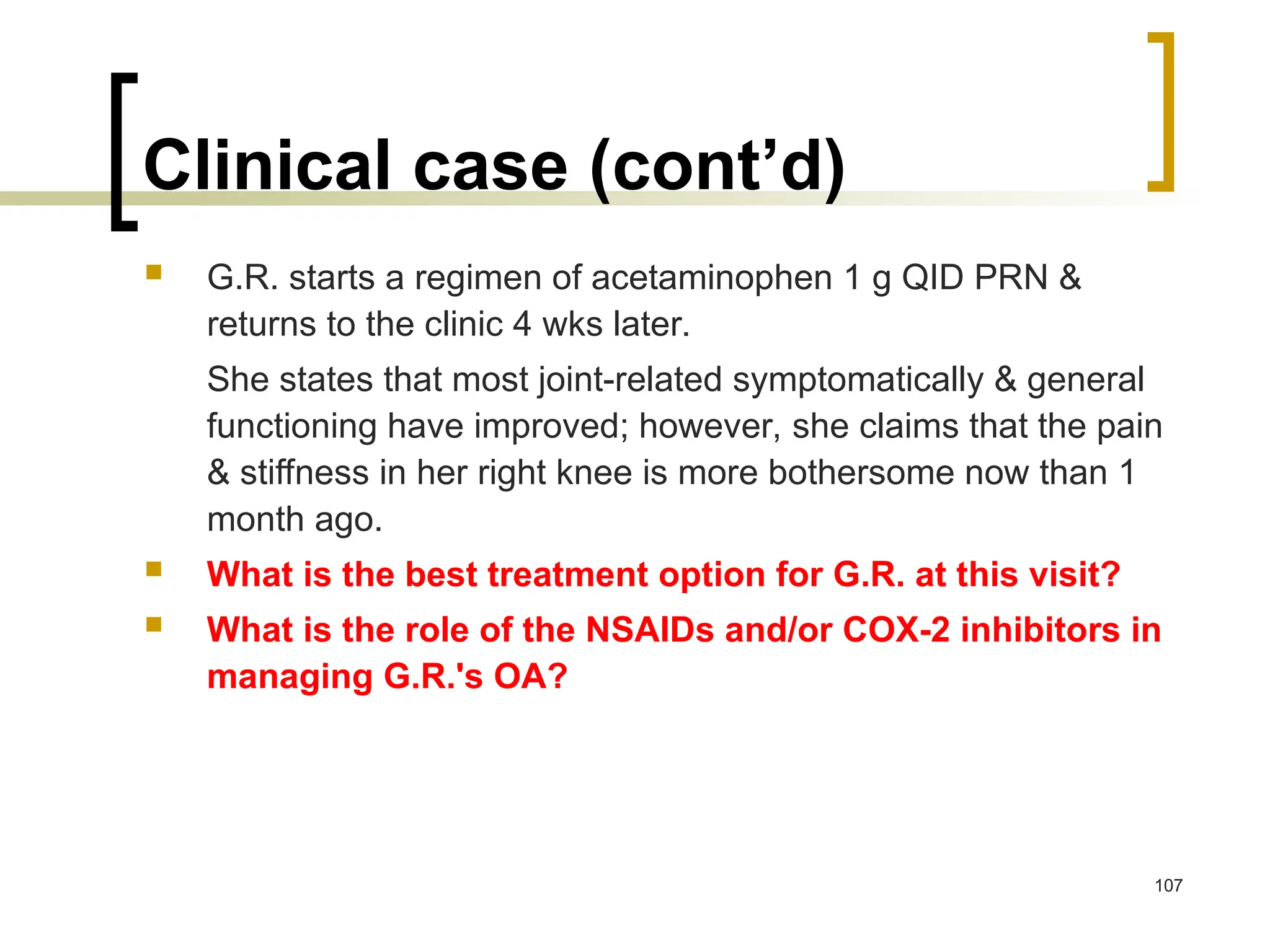
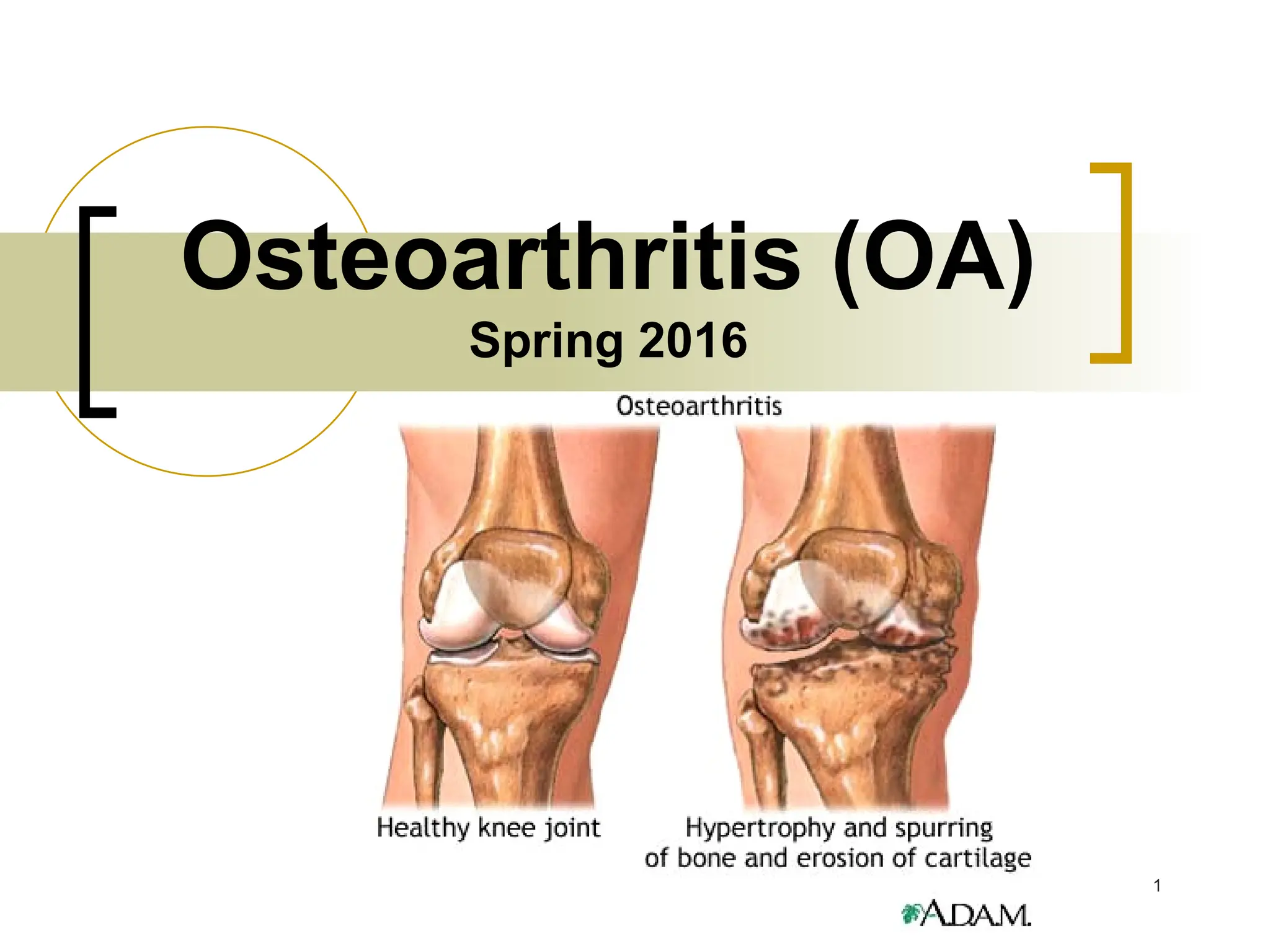
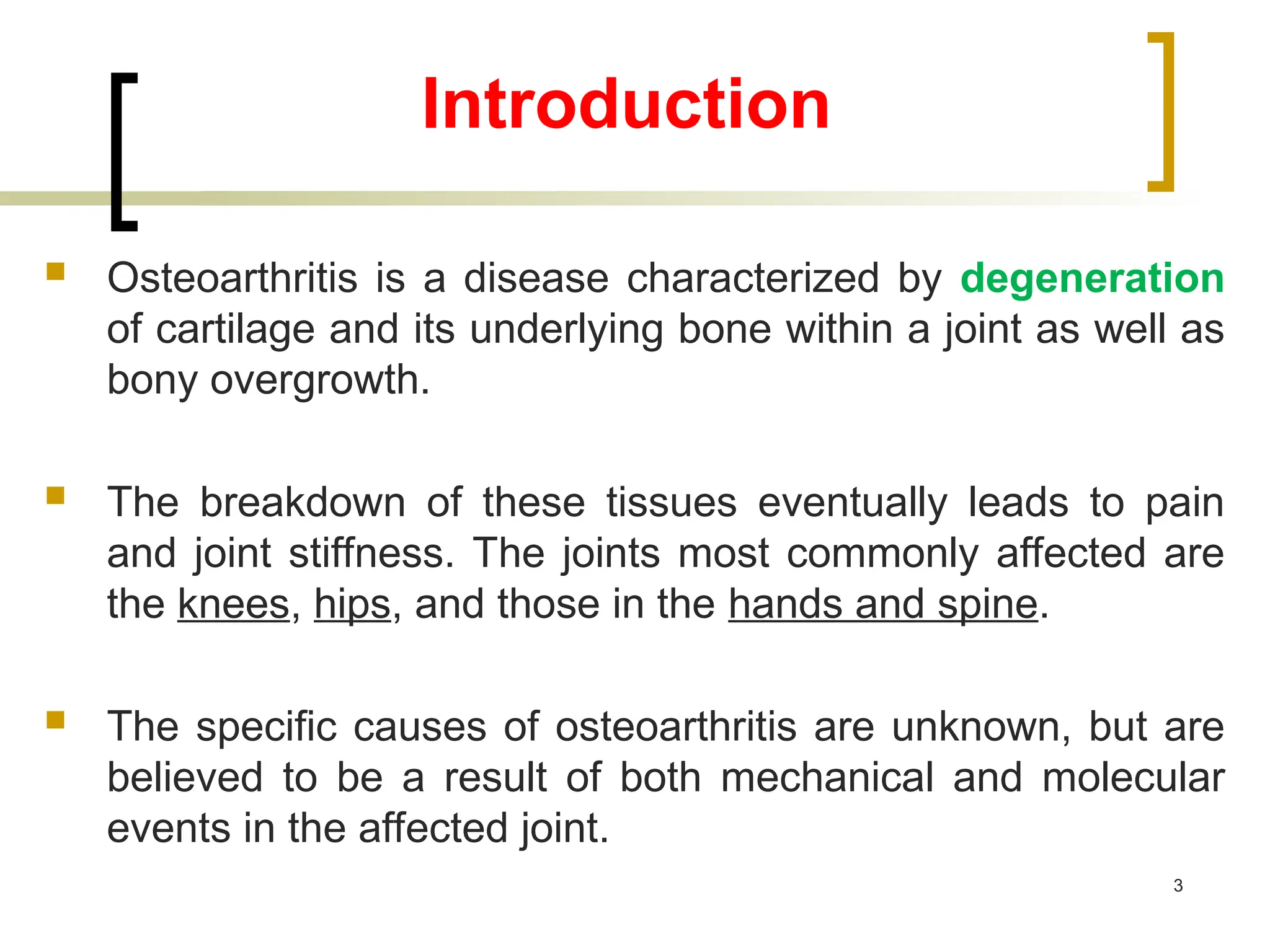
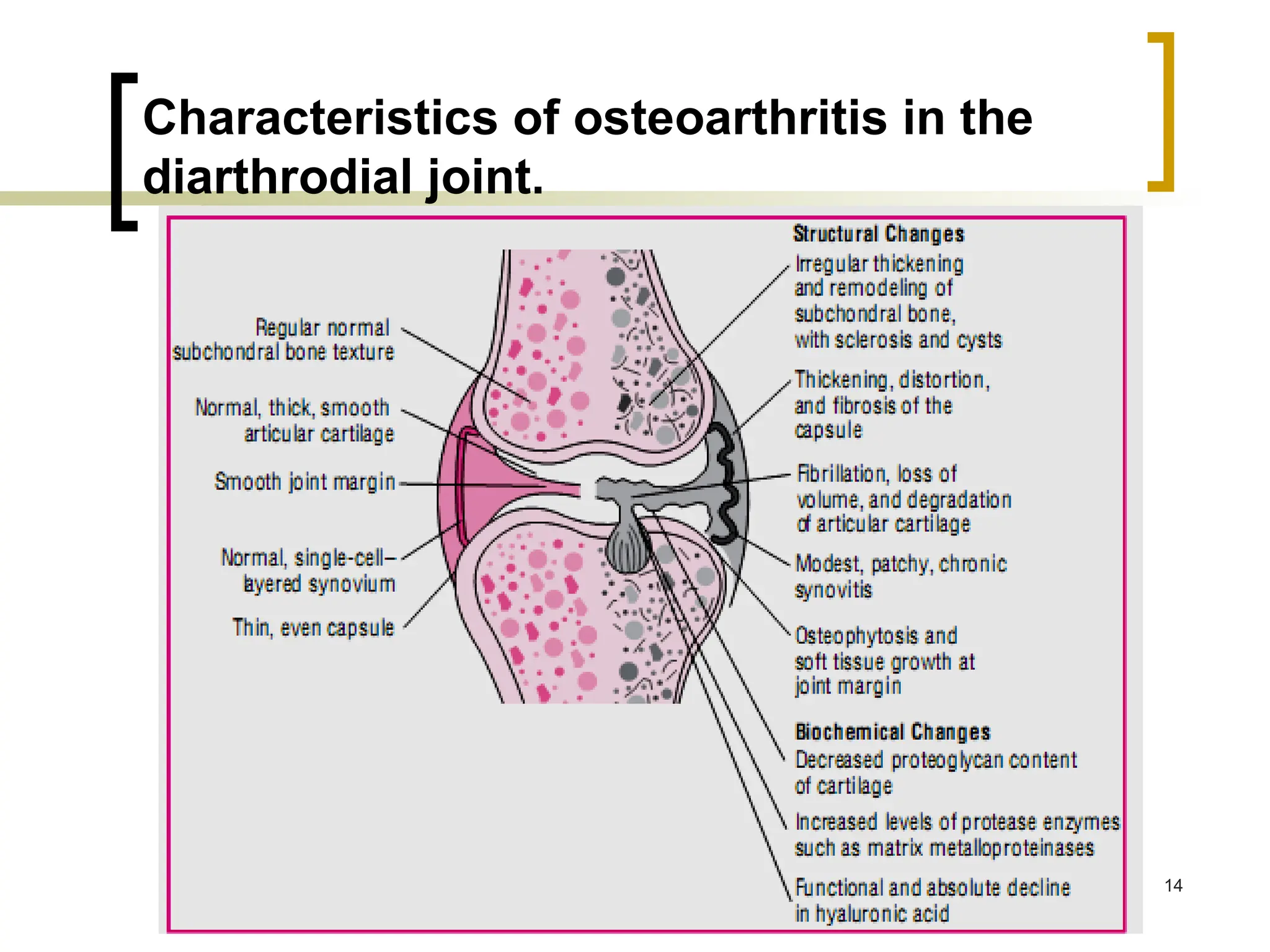
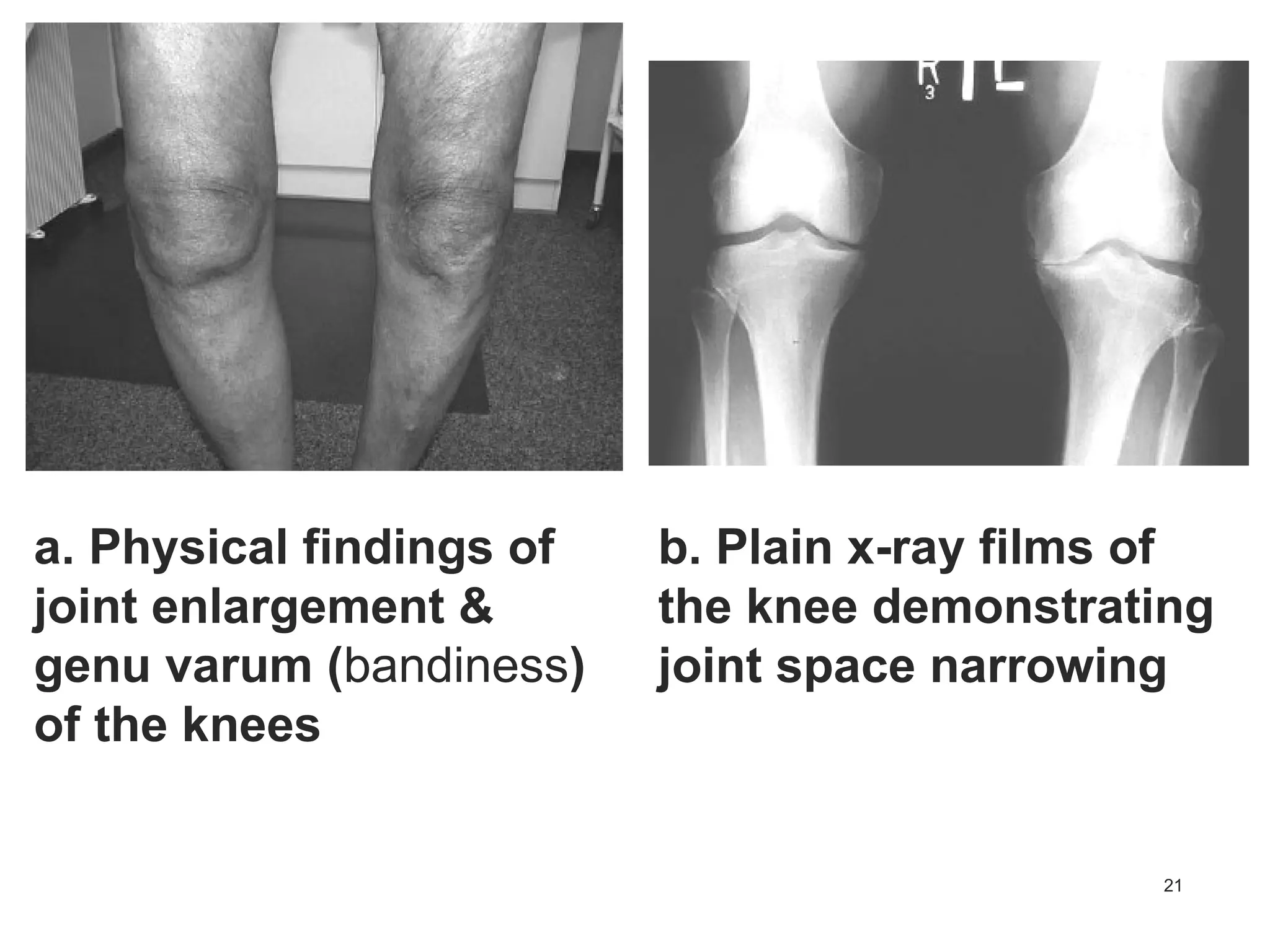
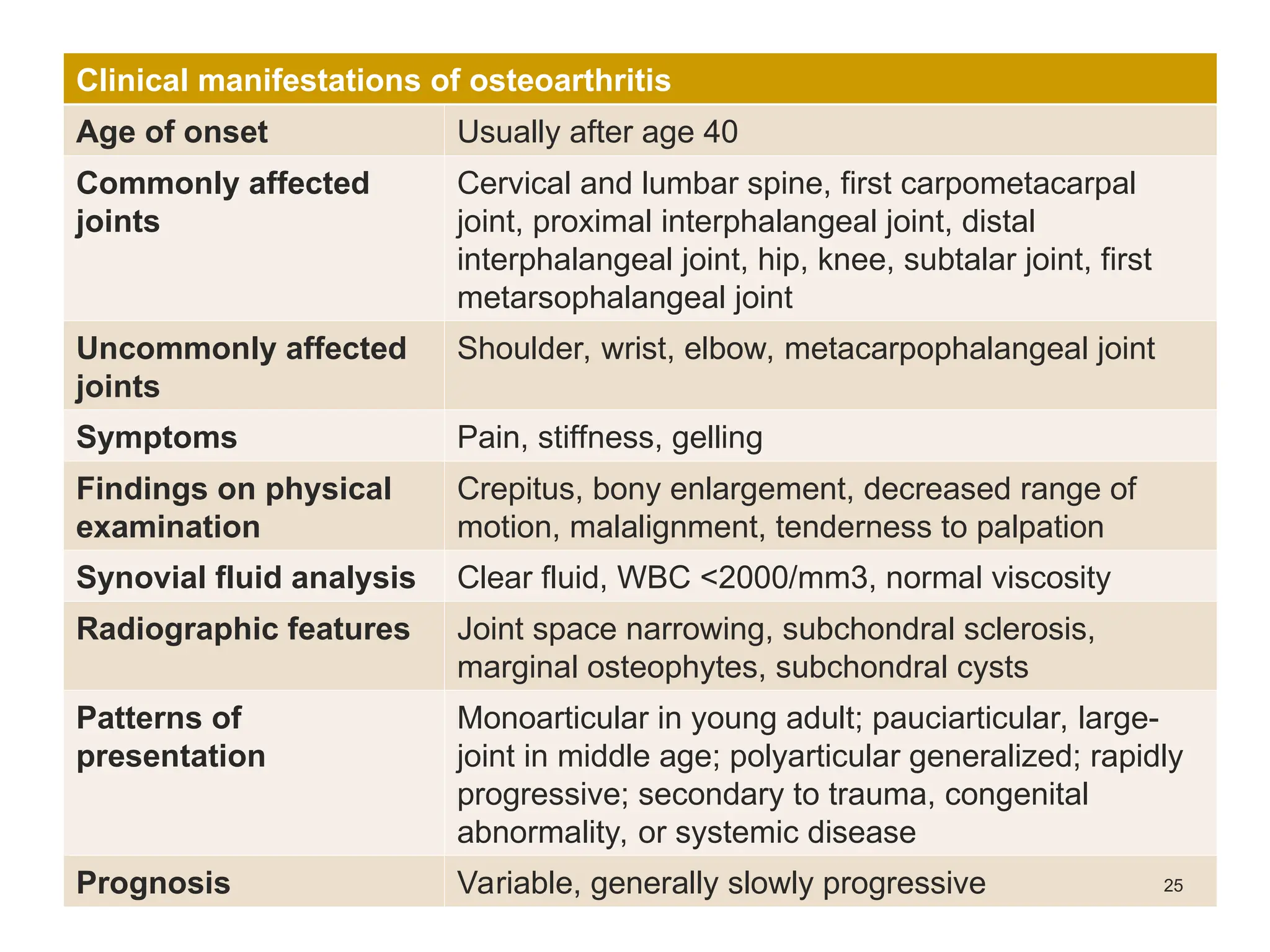
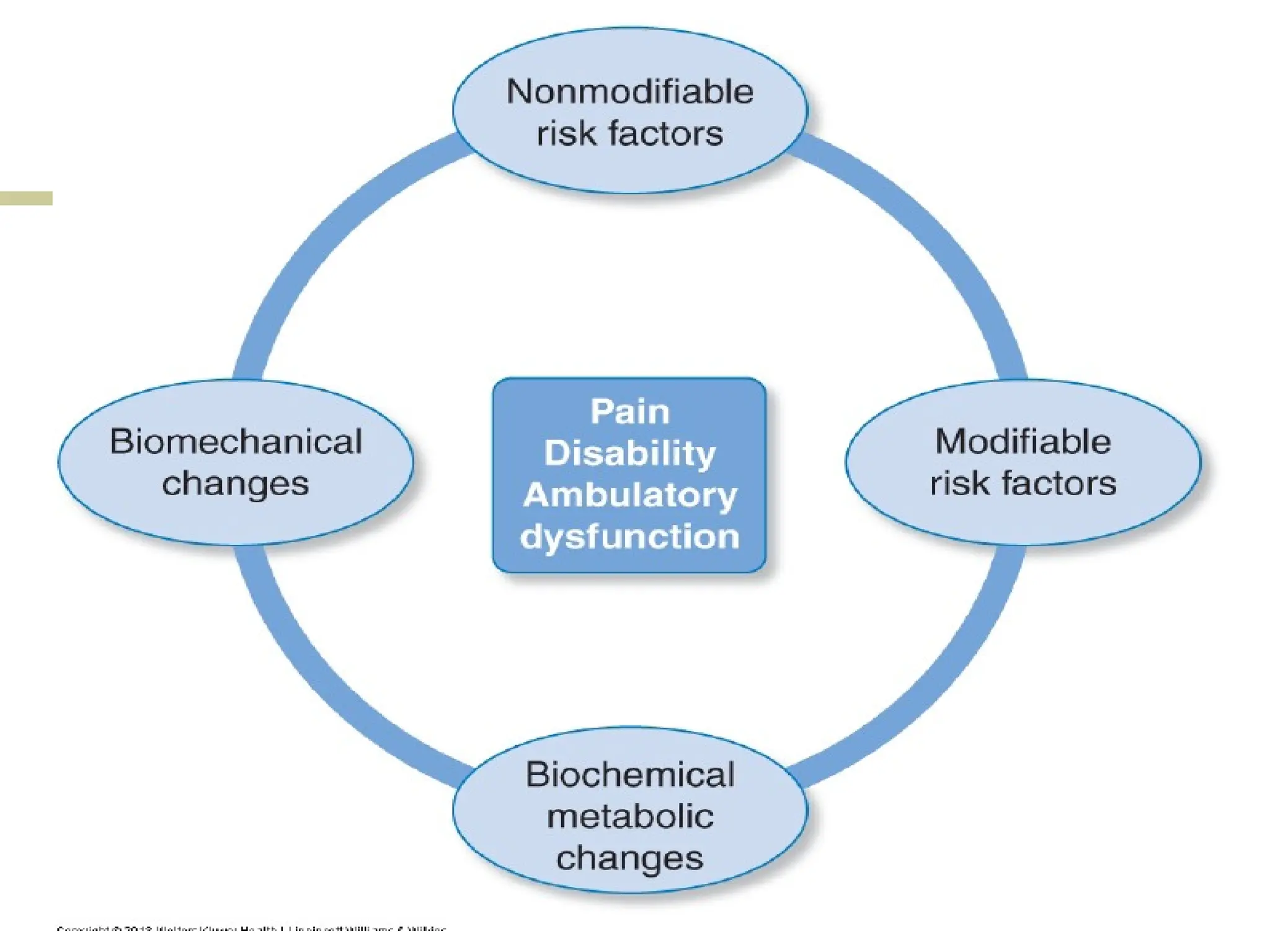
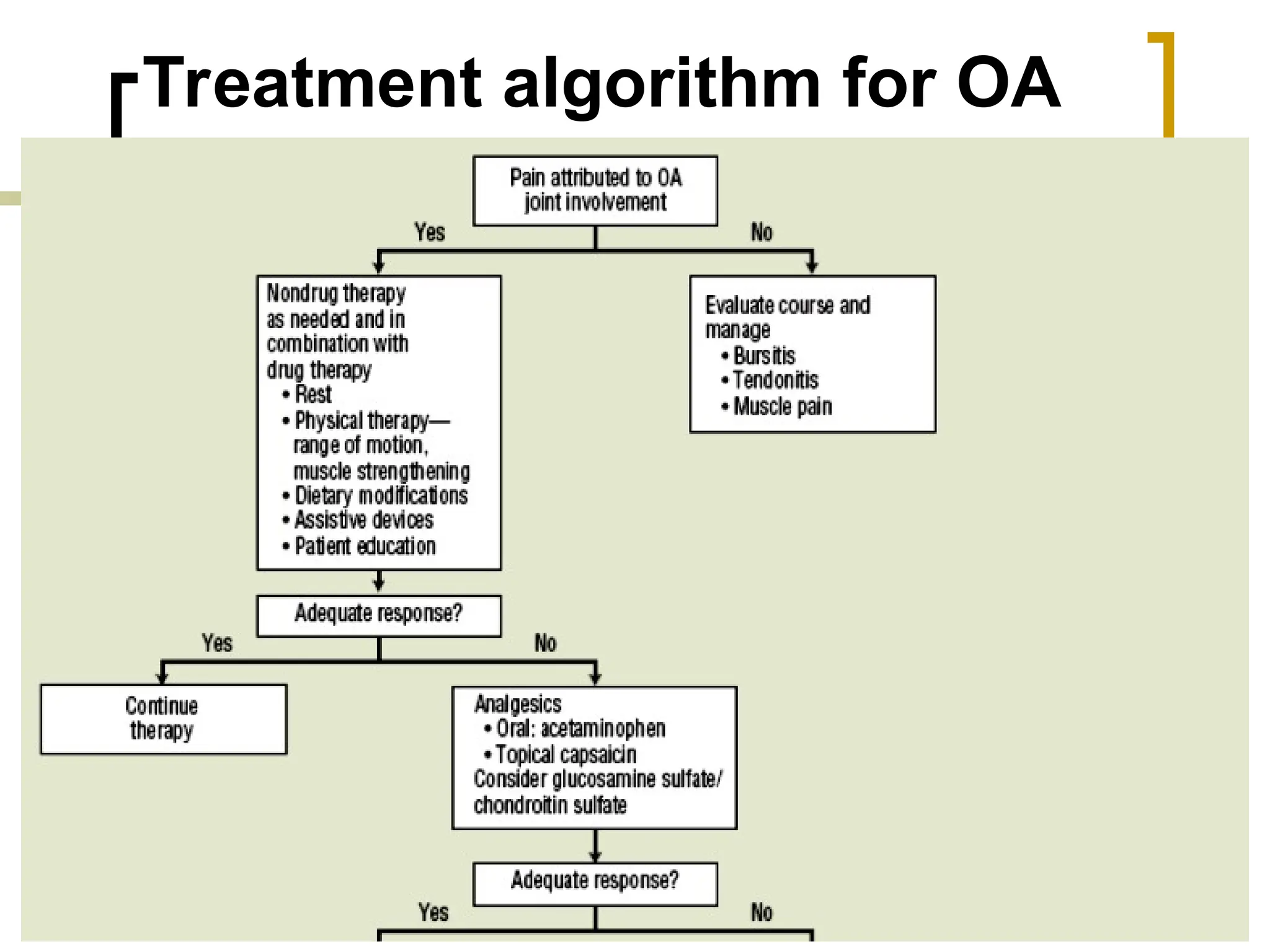
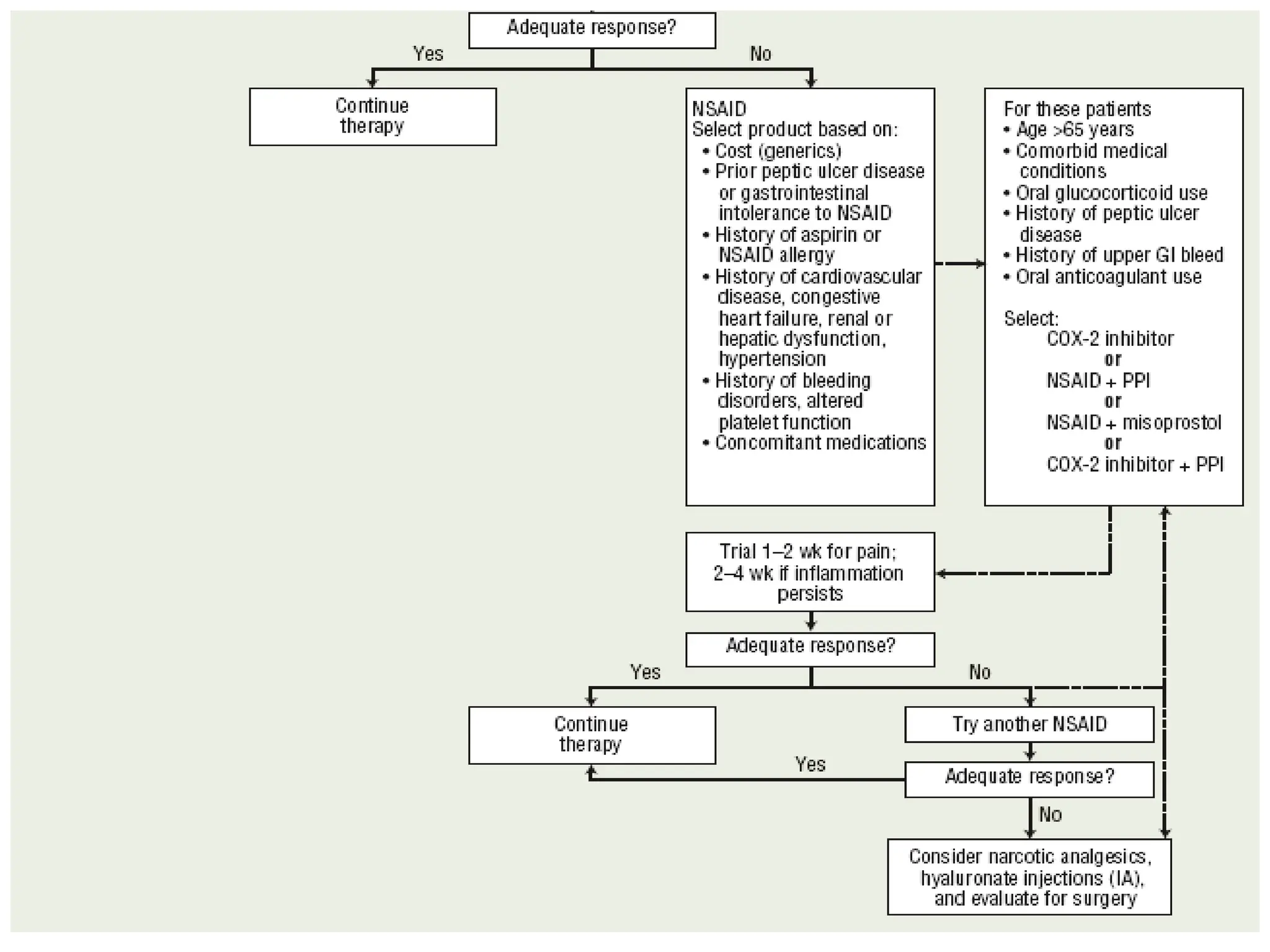
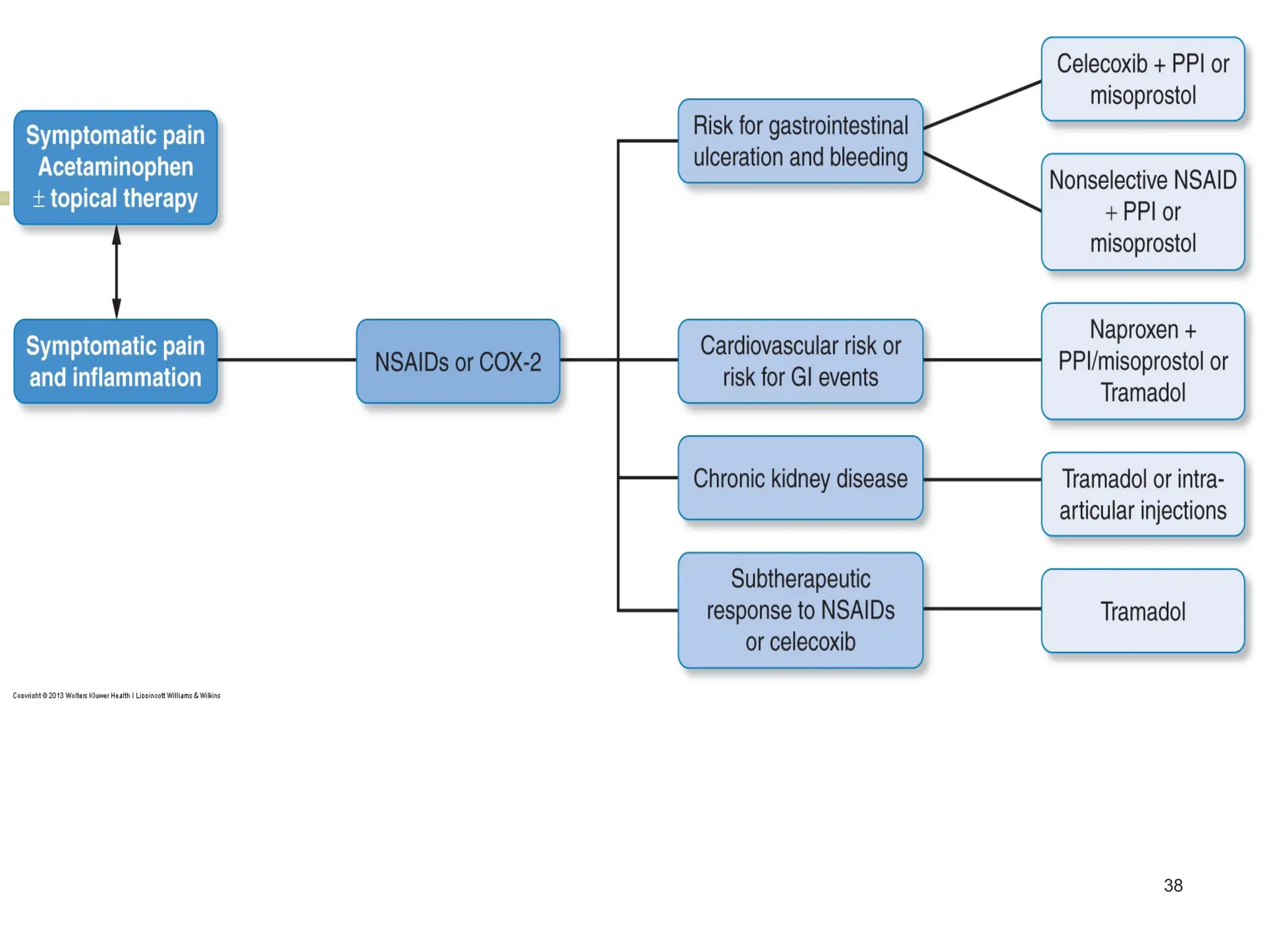
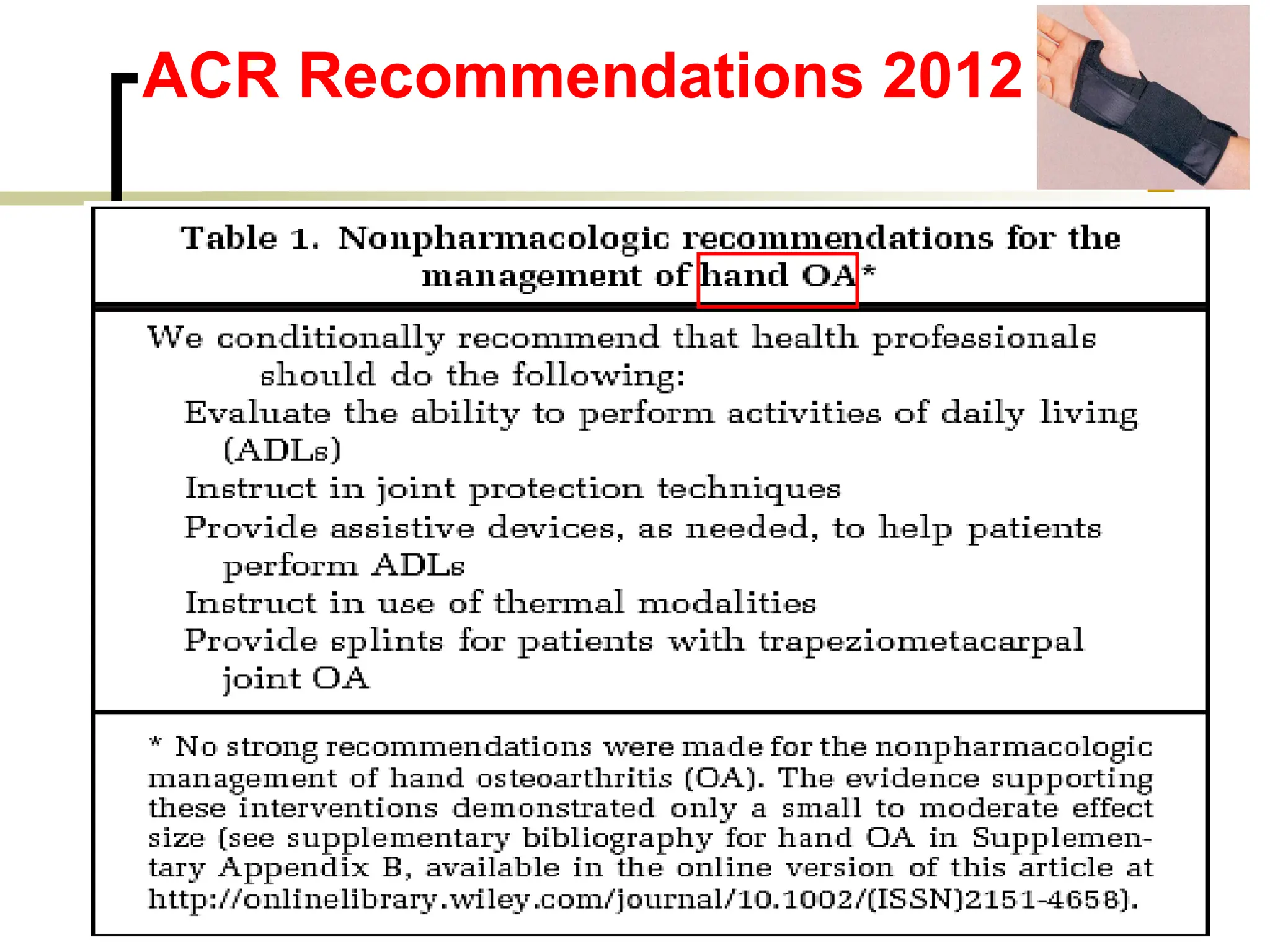
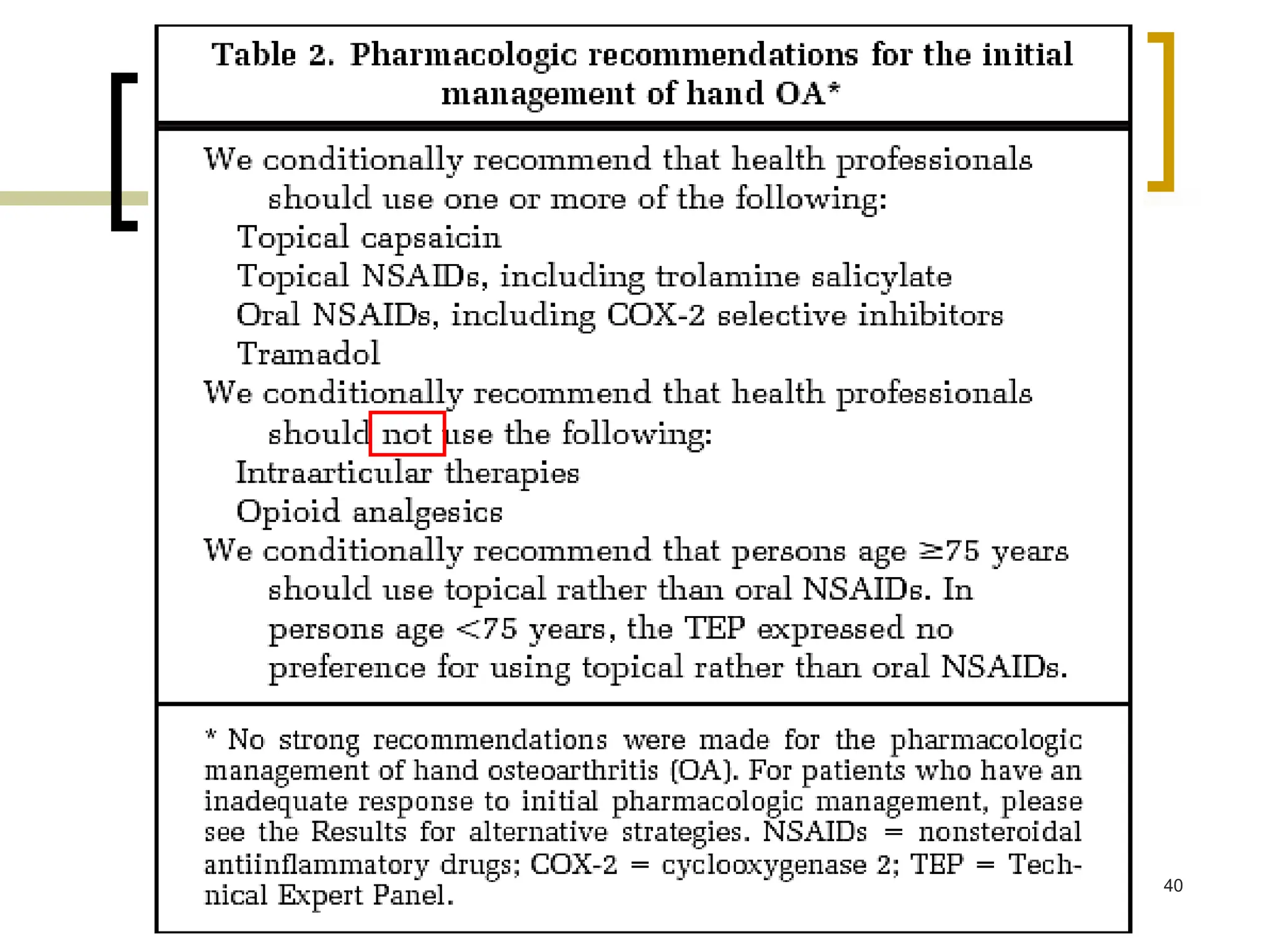
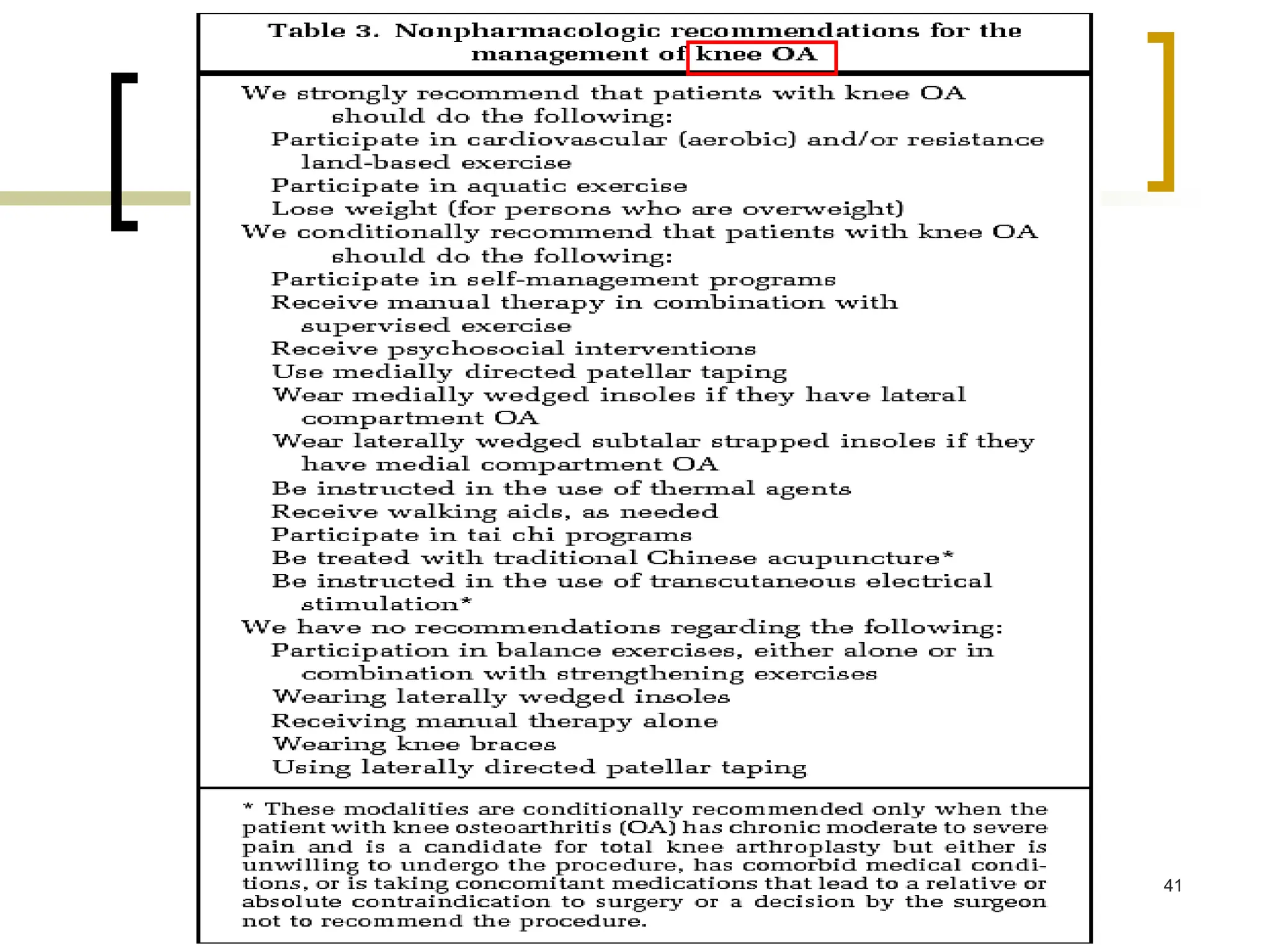
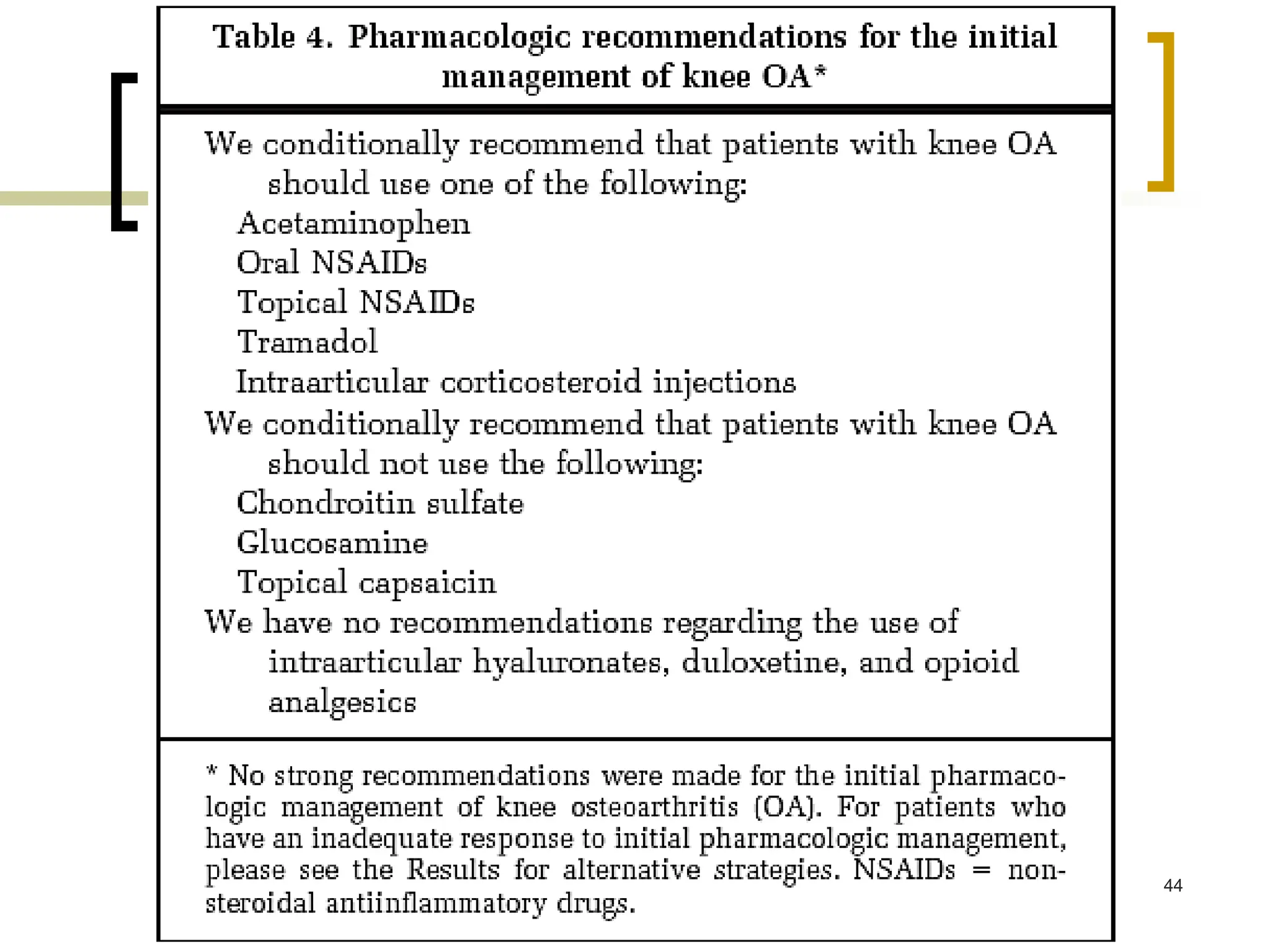
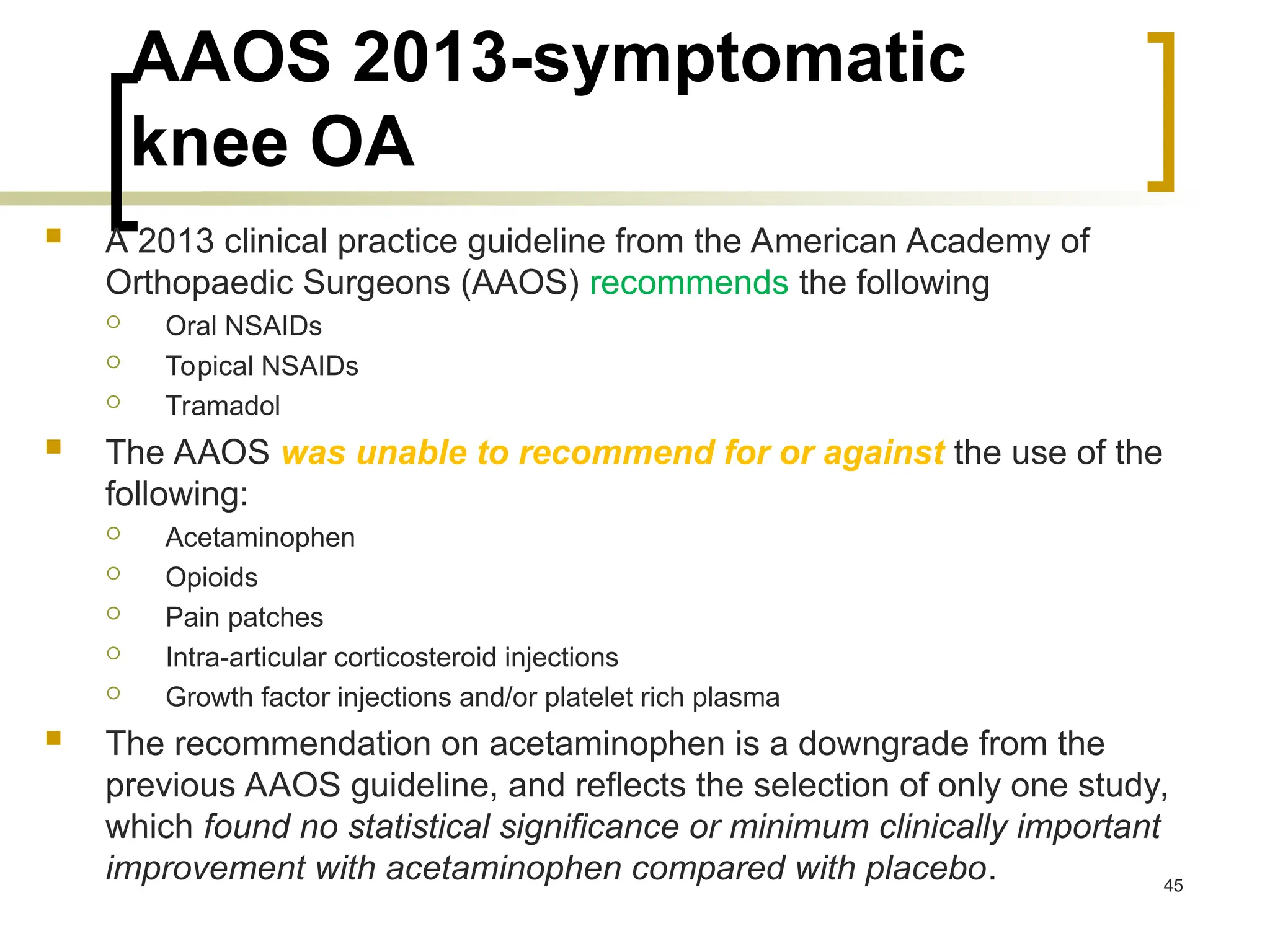
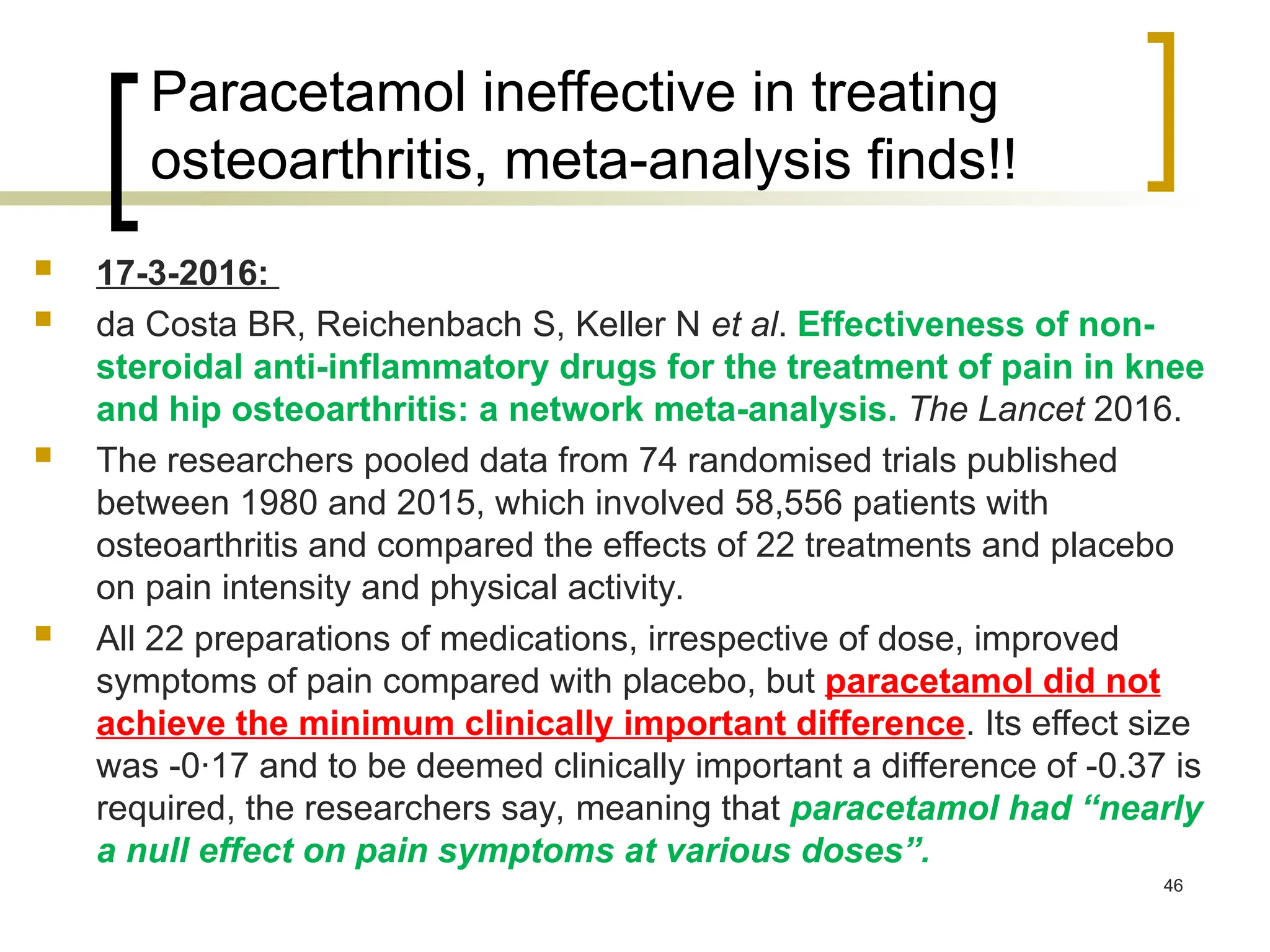
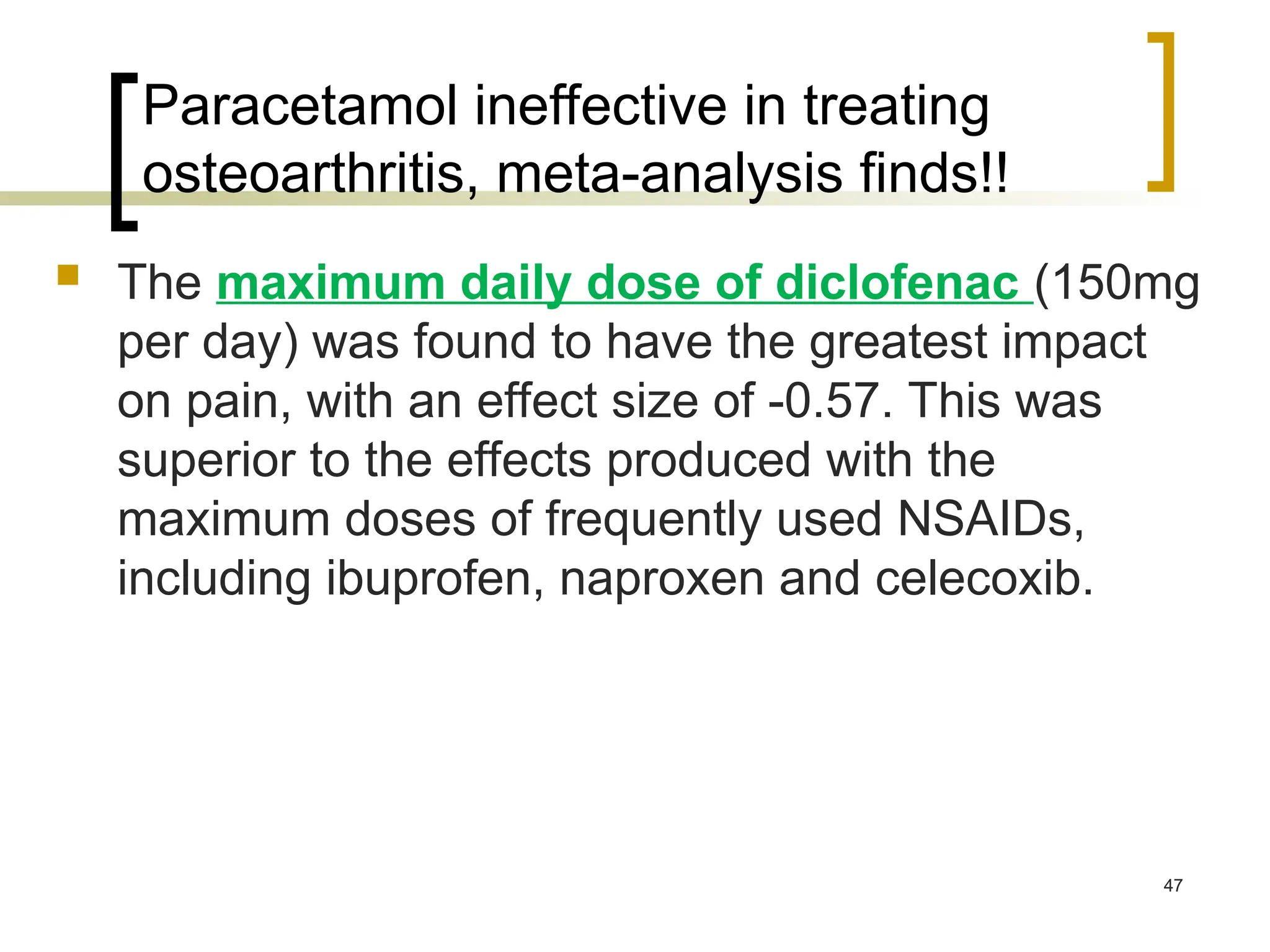
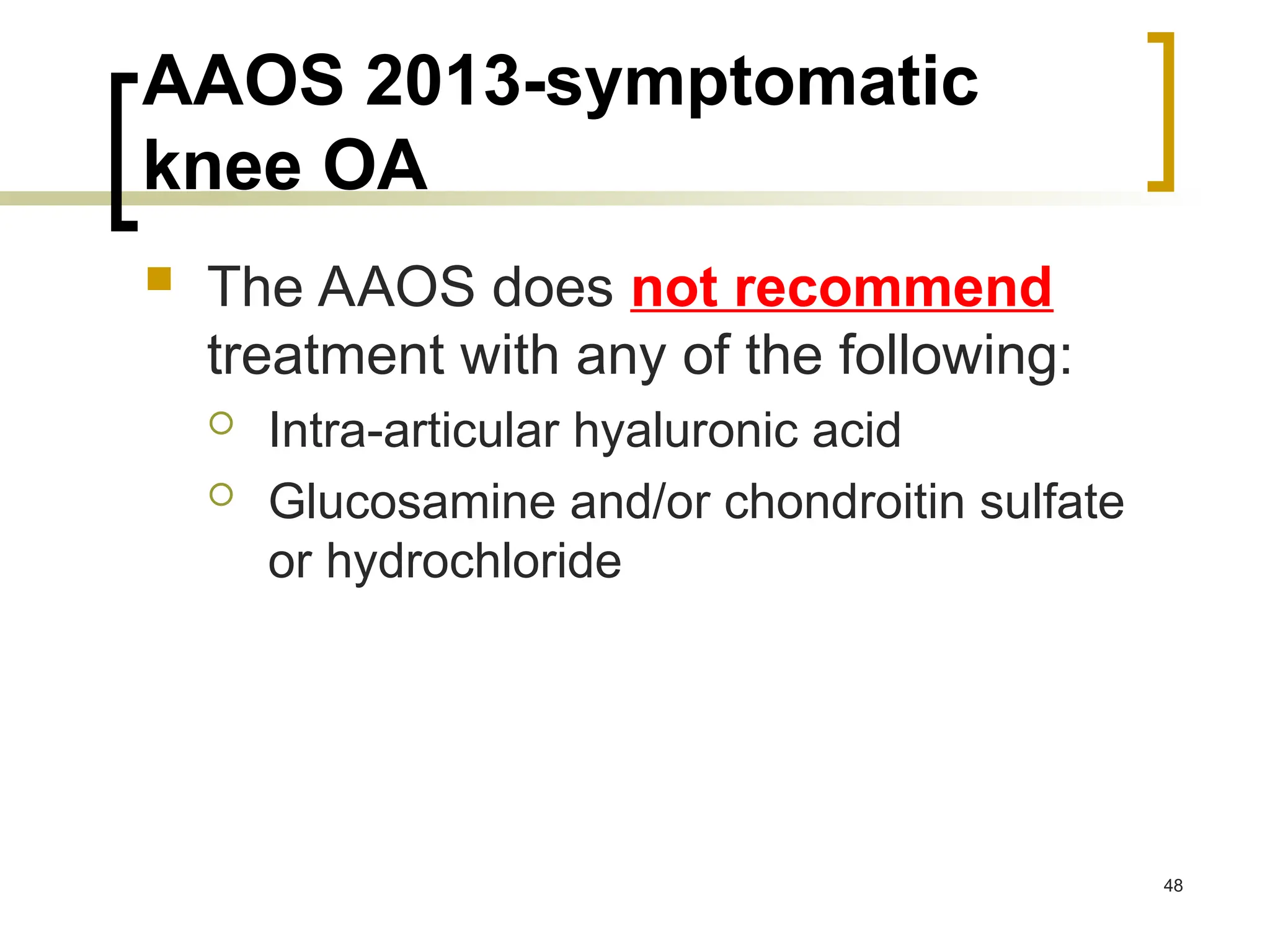
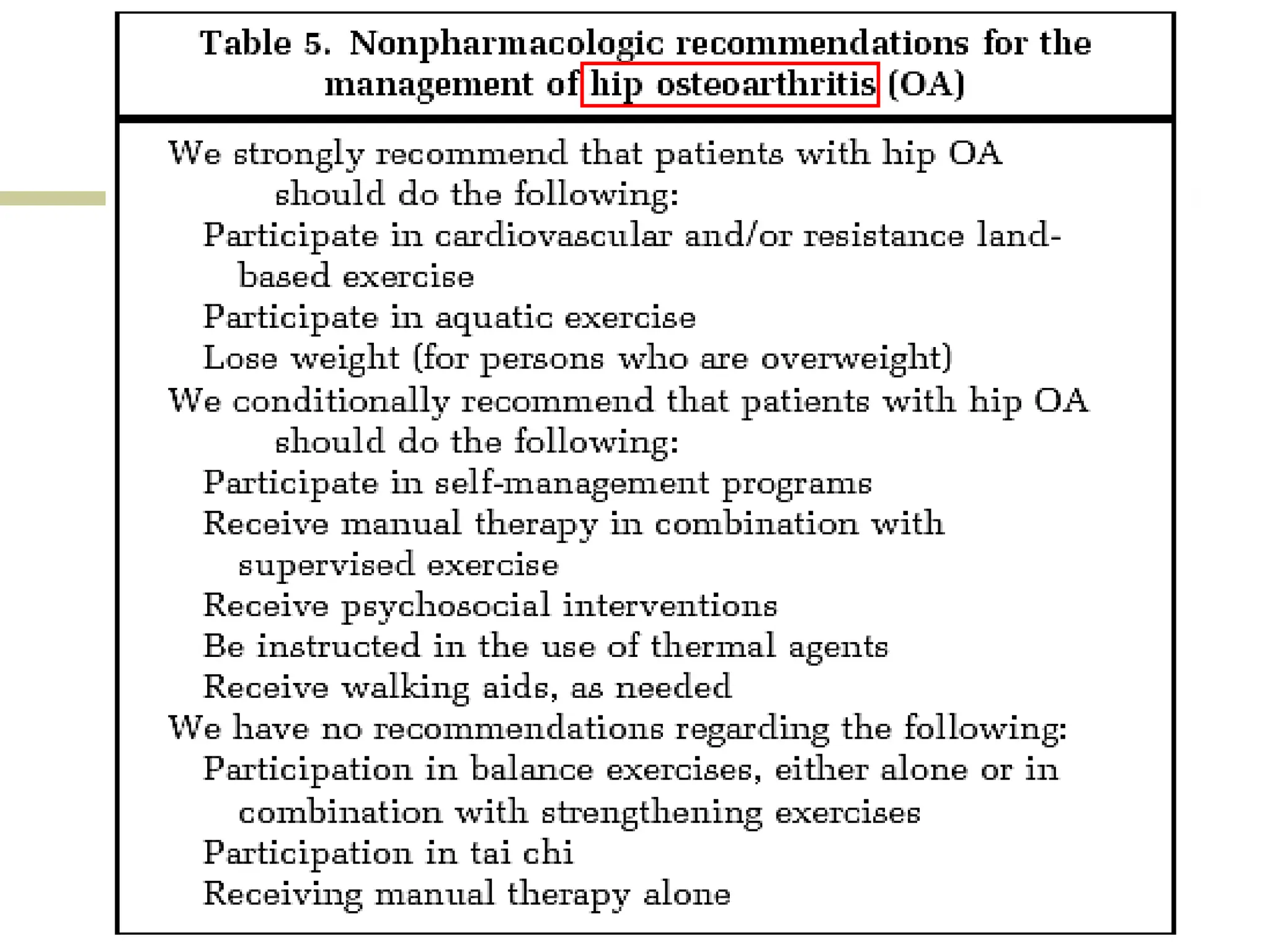
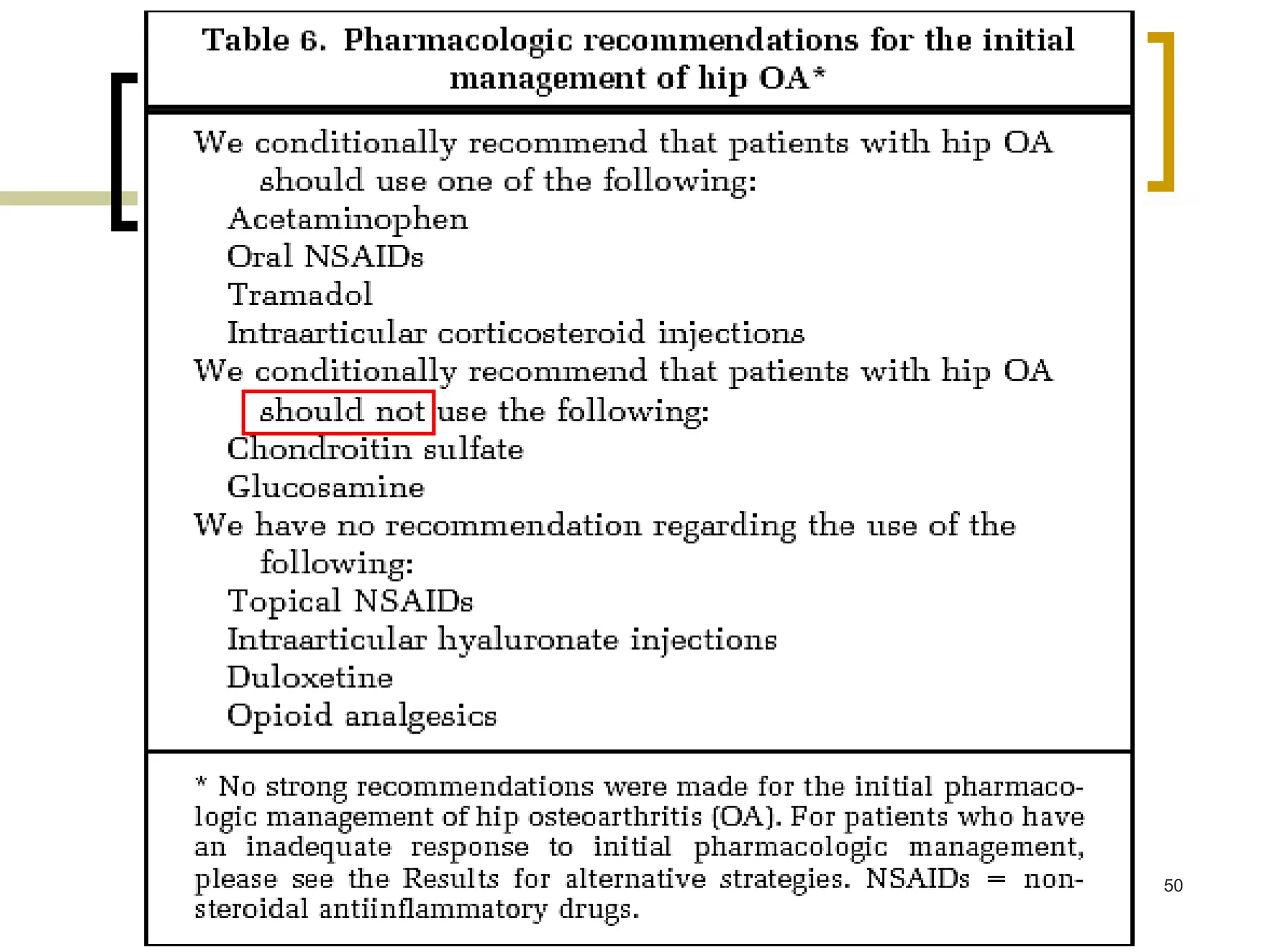
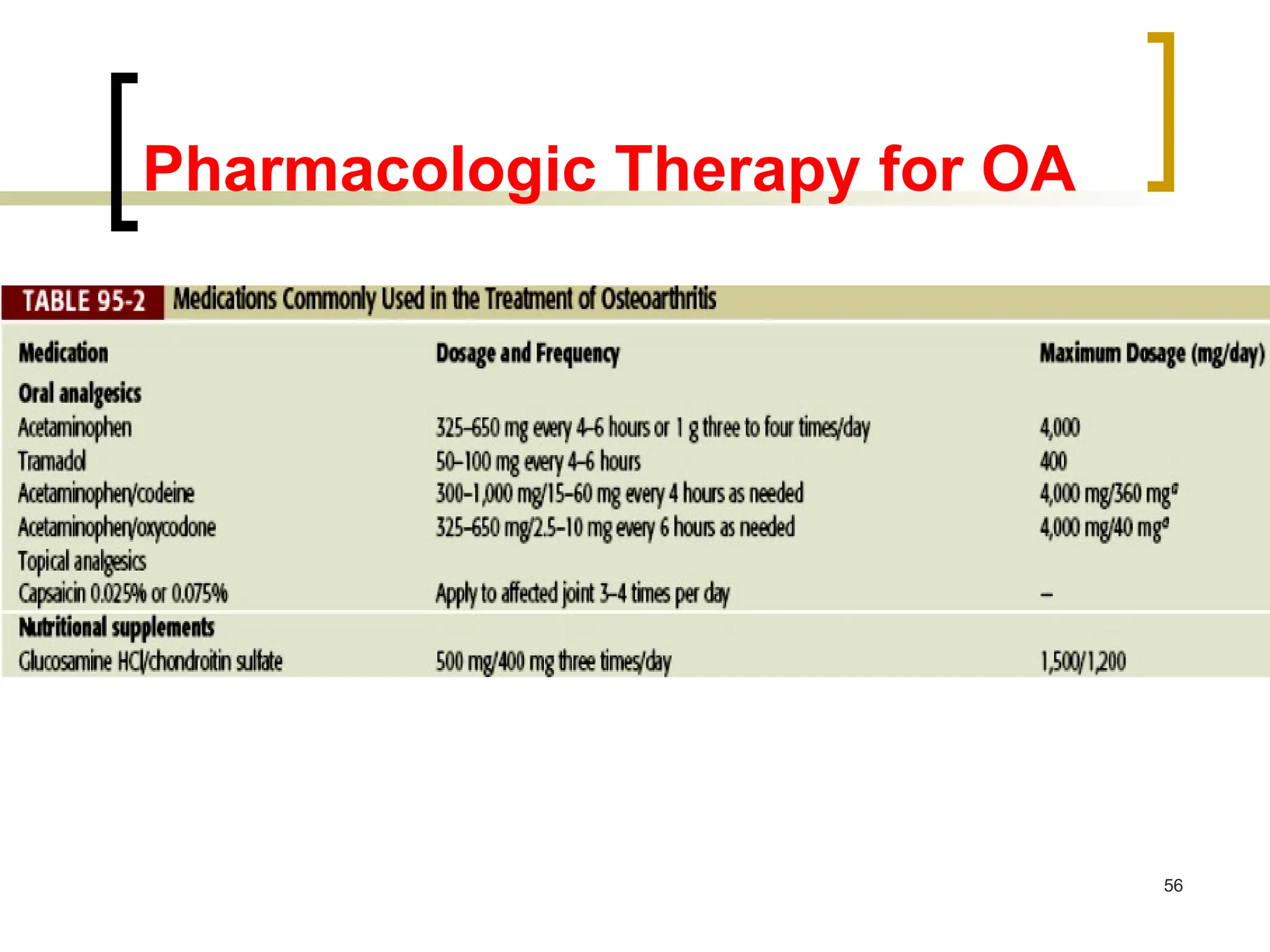
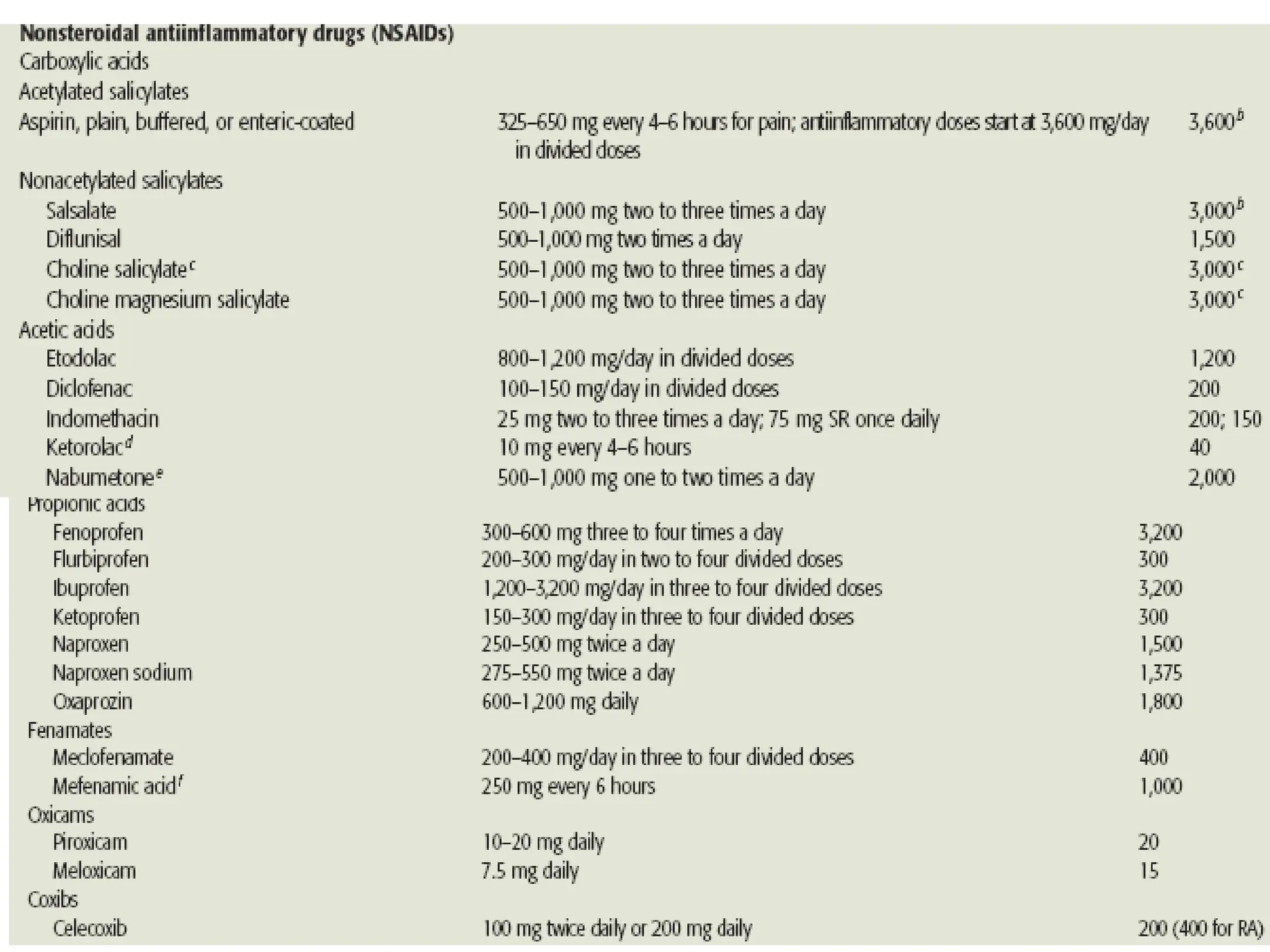
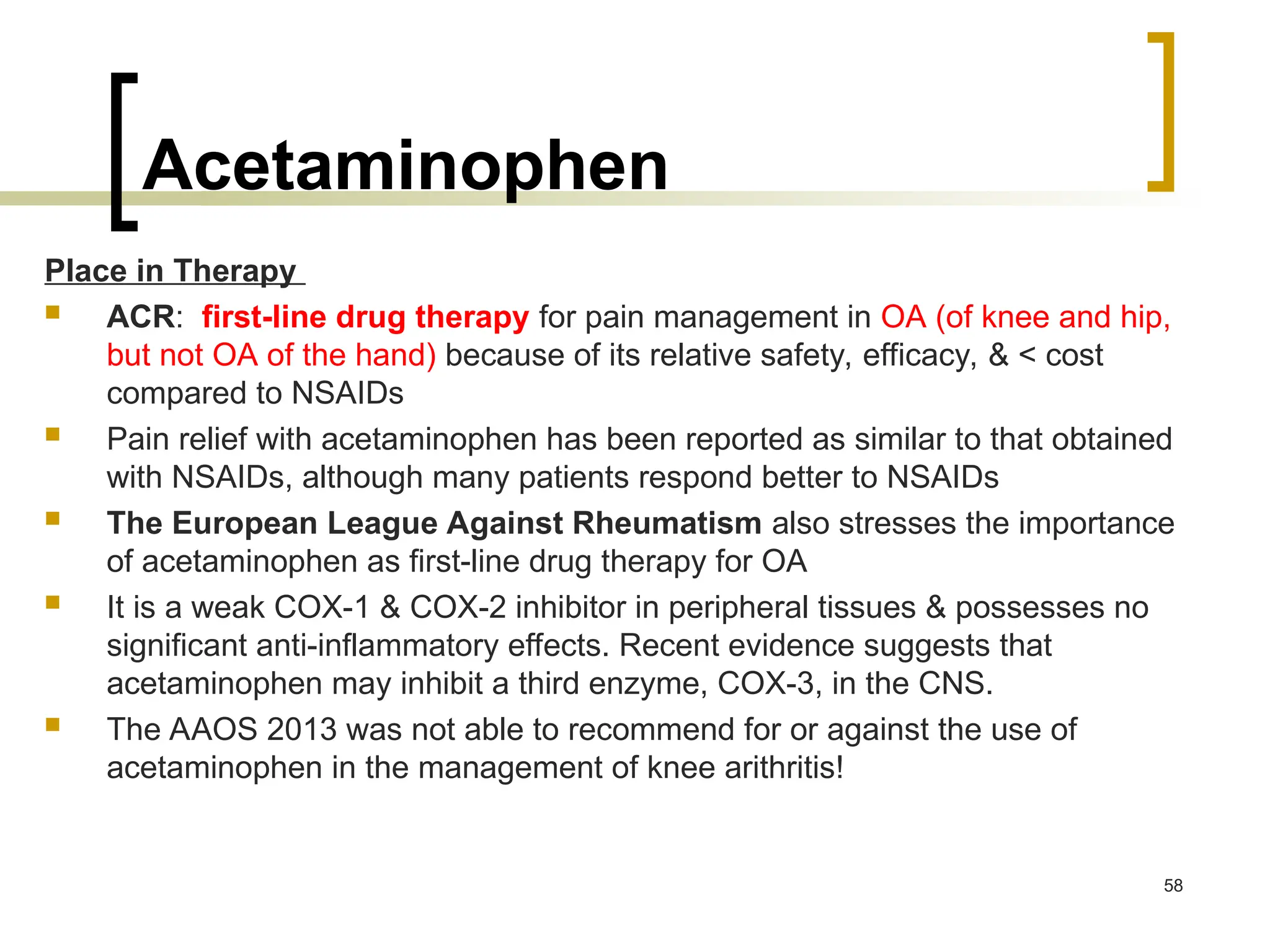
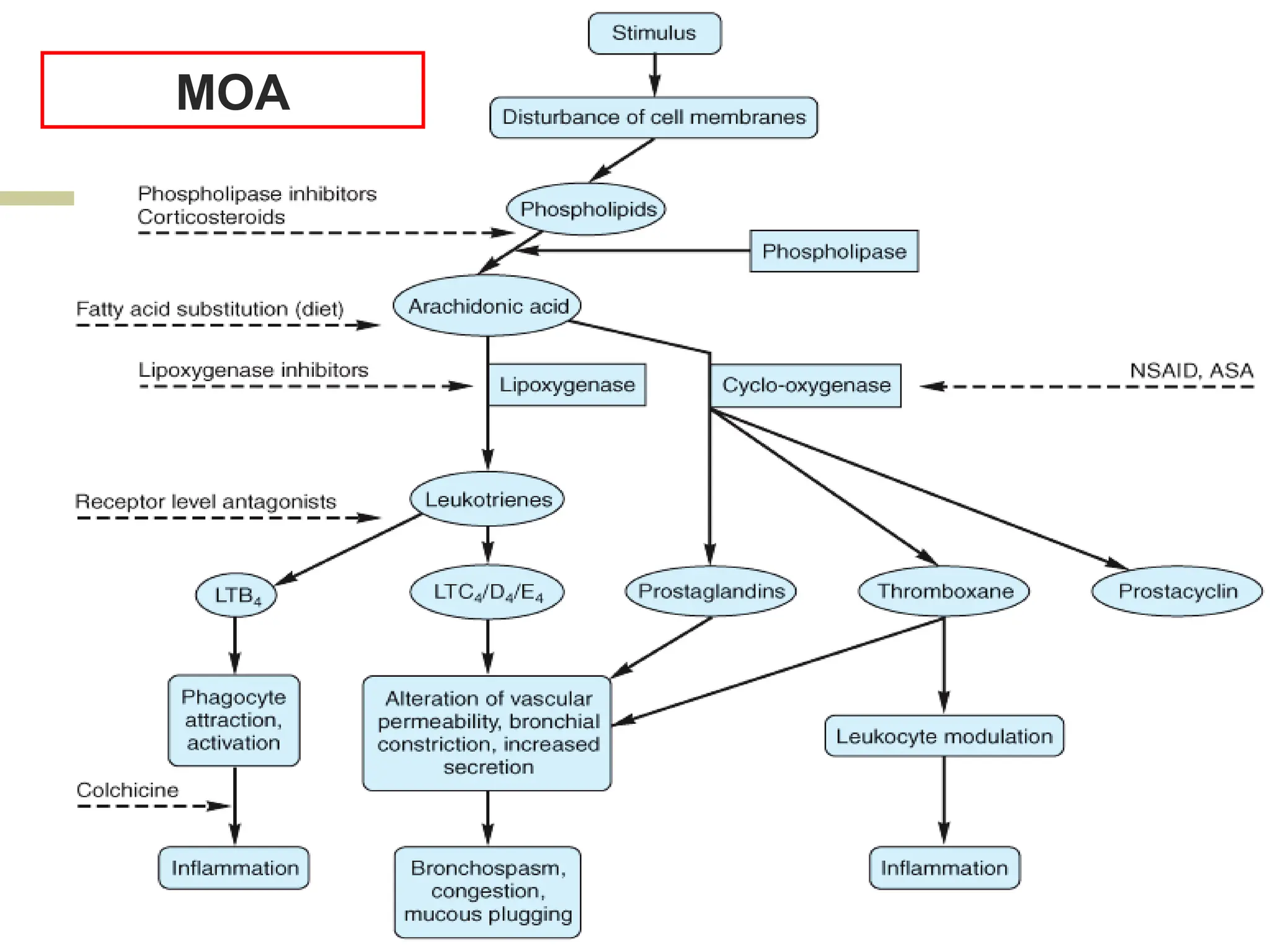
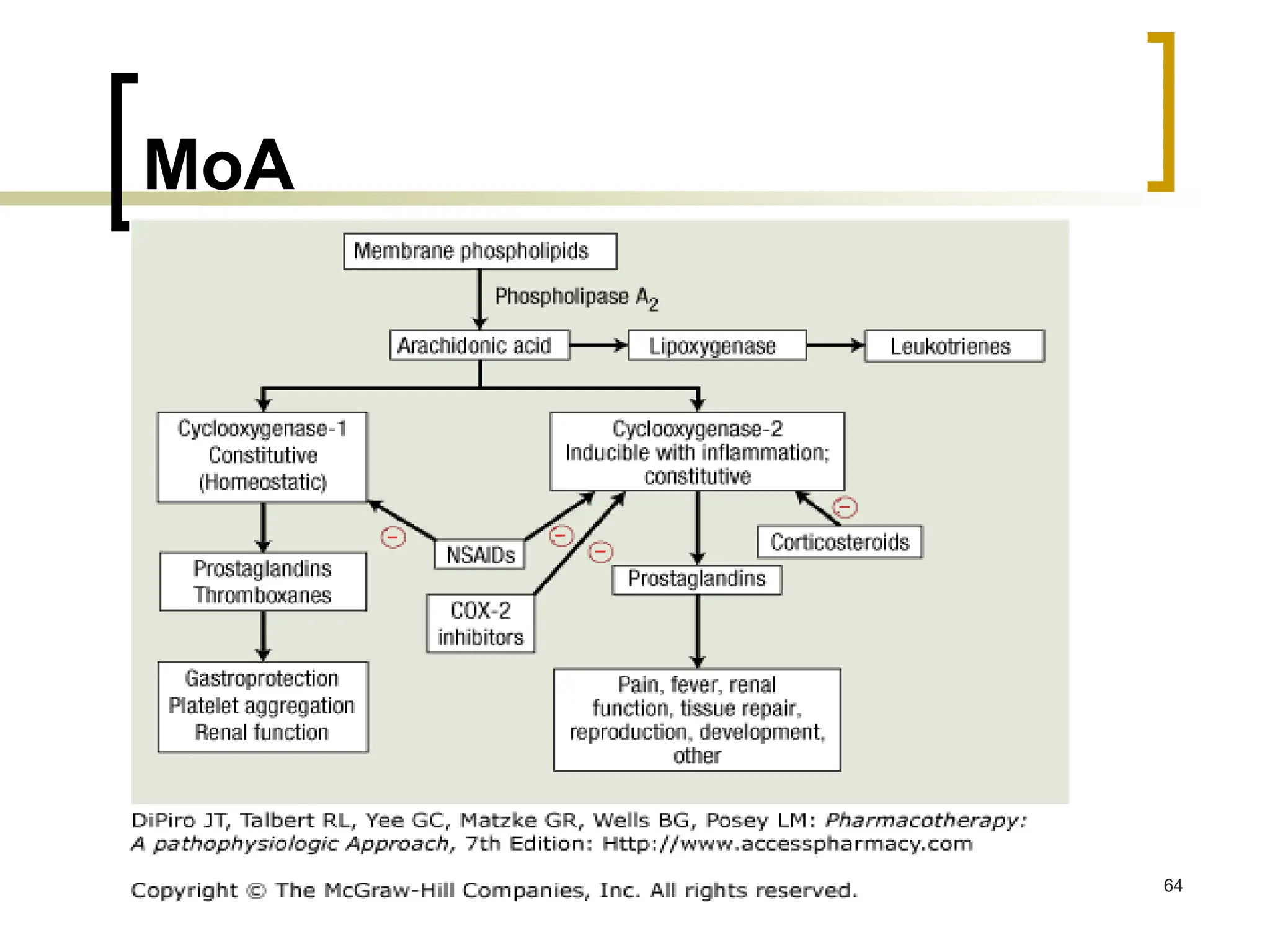
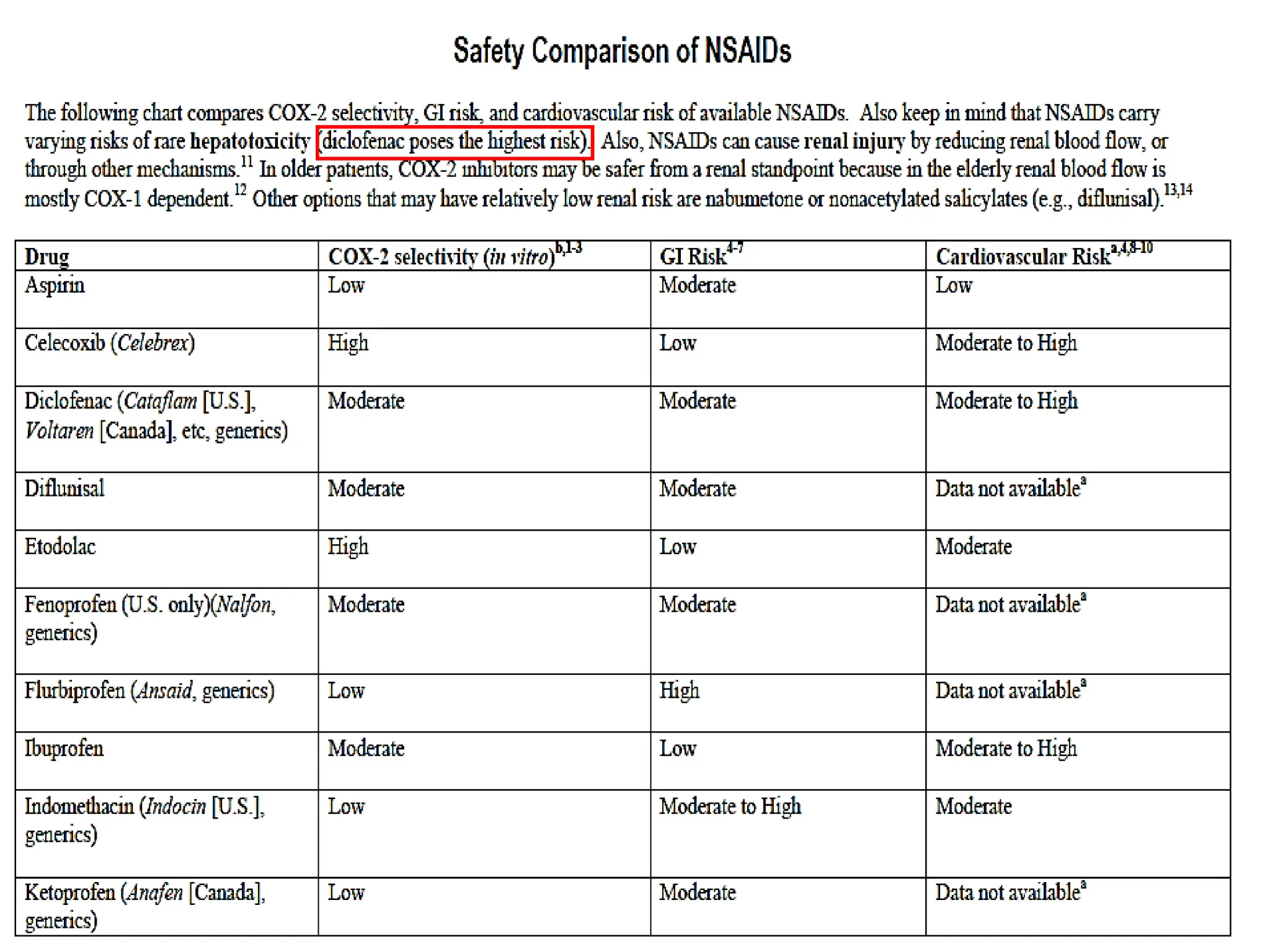
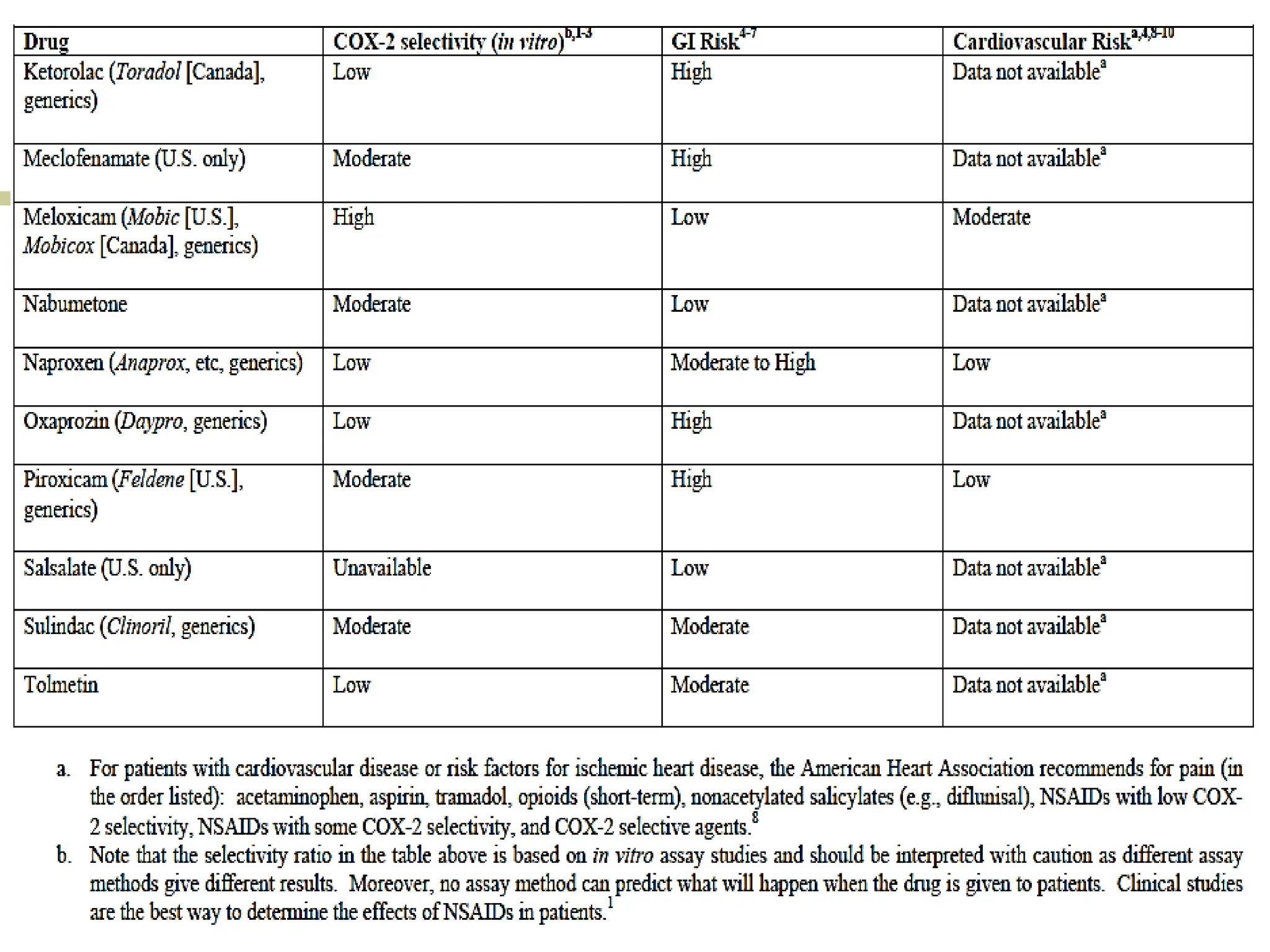
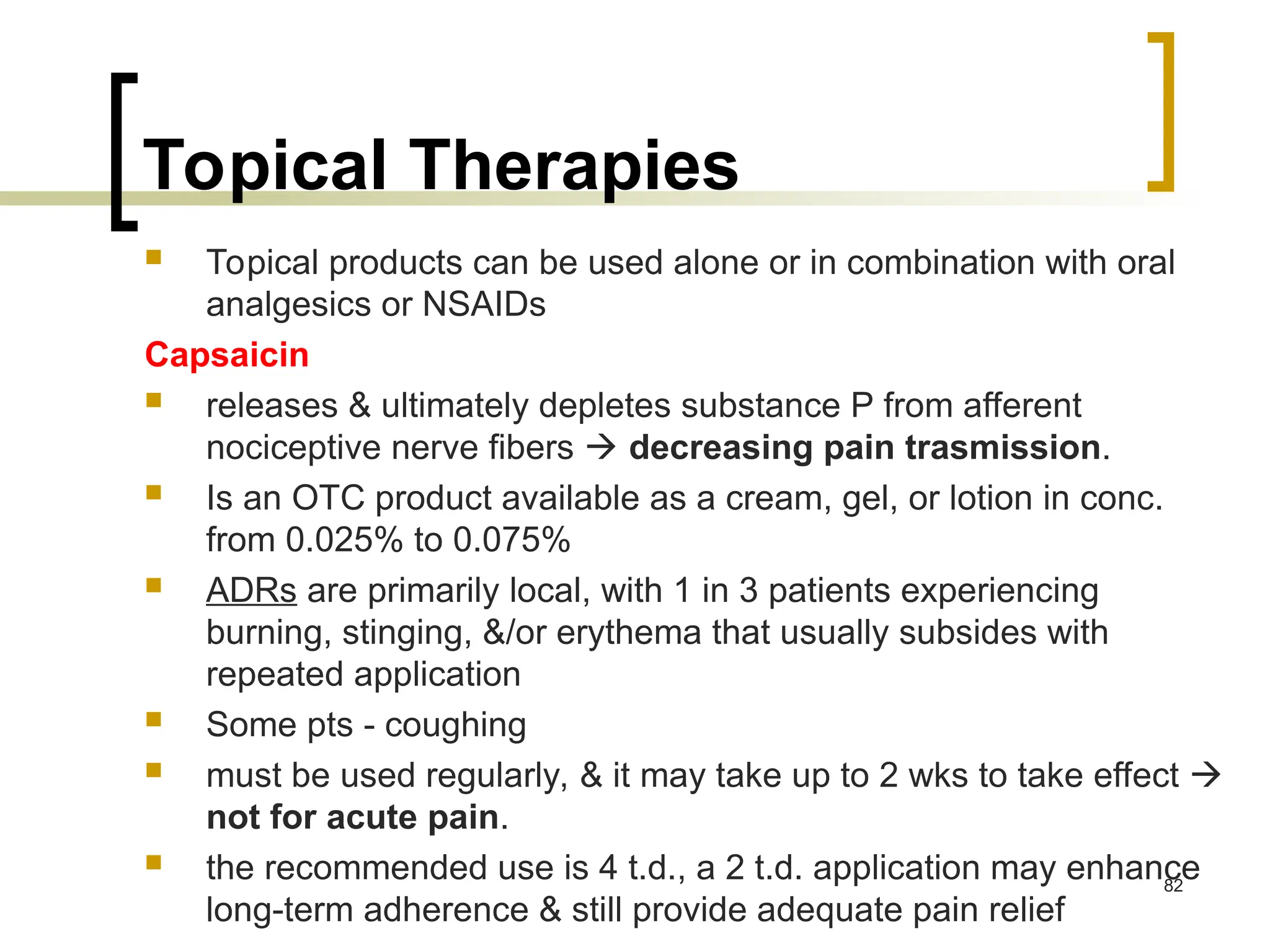
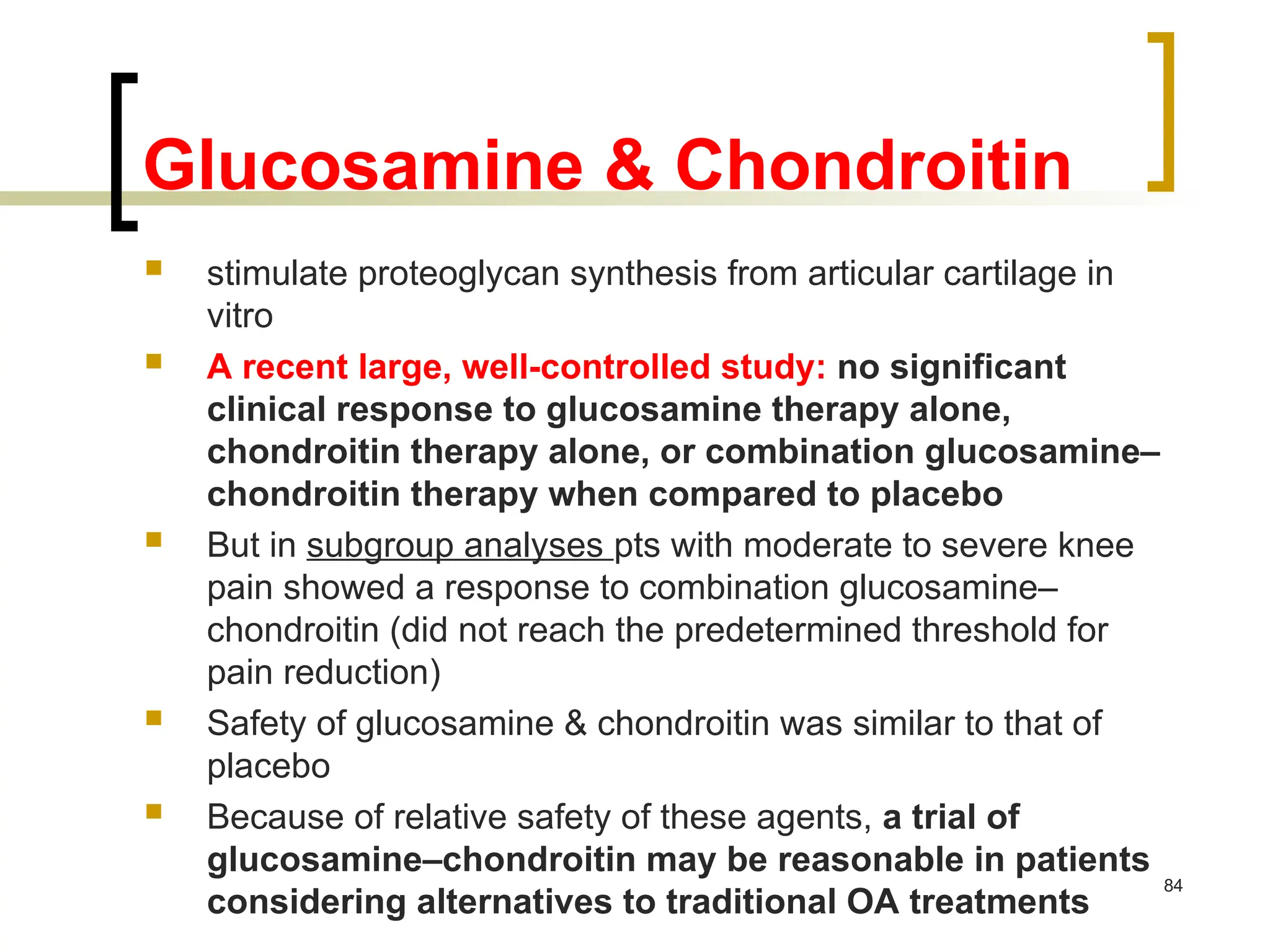
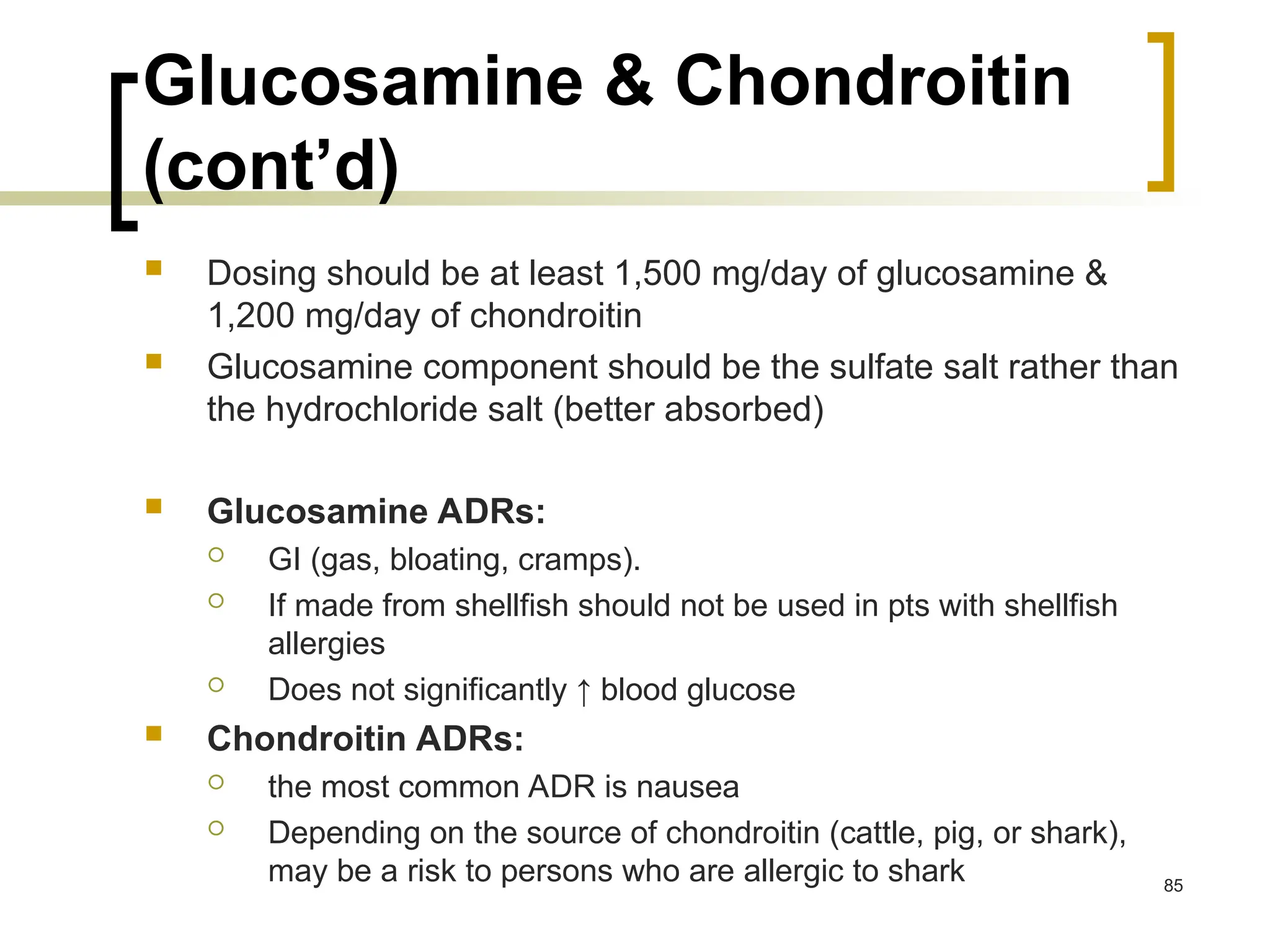
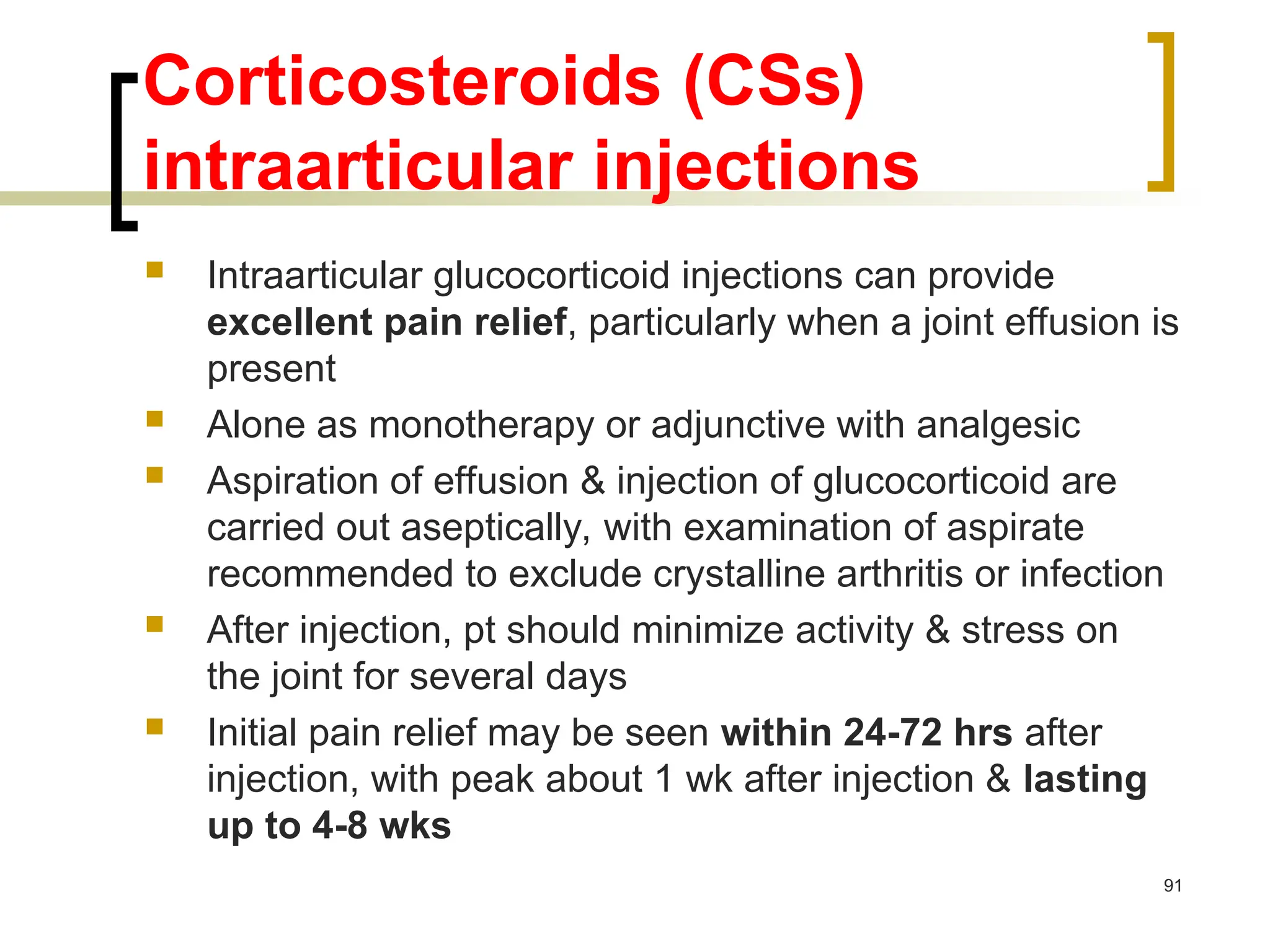
Osteoarthritis (OA) is a common degenerative joint disease characterized by cartilage degradation and bone overgrowth, leading to pain and stiffness, especially in the knees, hips, and hands. Although the exact causes are unknown, risk factors include aging, obesity, and previous joint injuries, with no cure currently available; management focuses on symptom relief through education, physical therapy, medications, and potentially joint replacement. Treatment recommendations suggest a combination of non-pharmacologic and pharmacologic approaches, with NSAIDs being commonly used for pain relief.



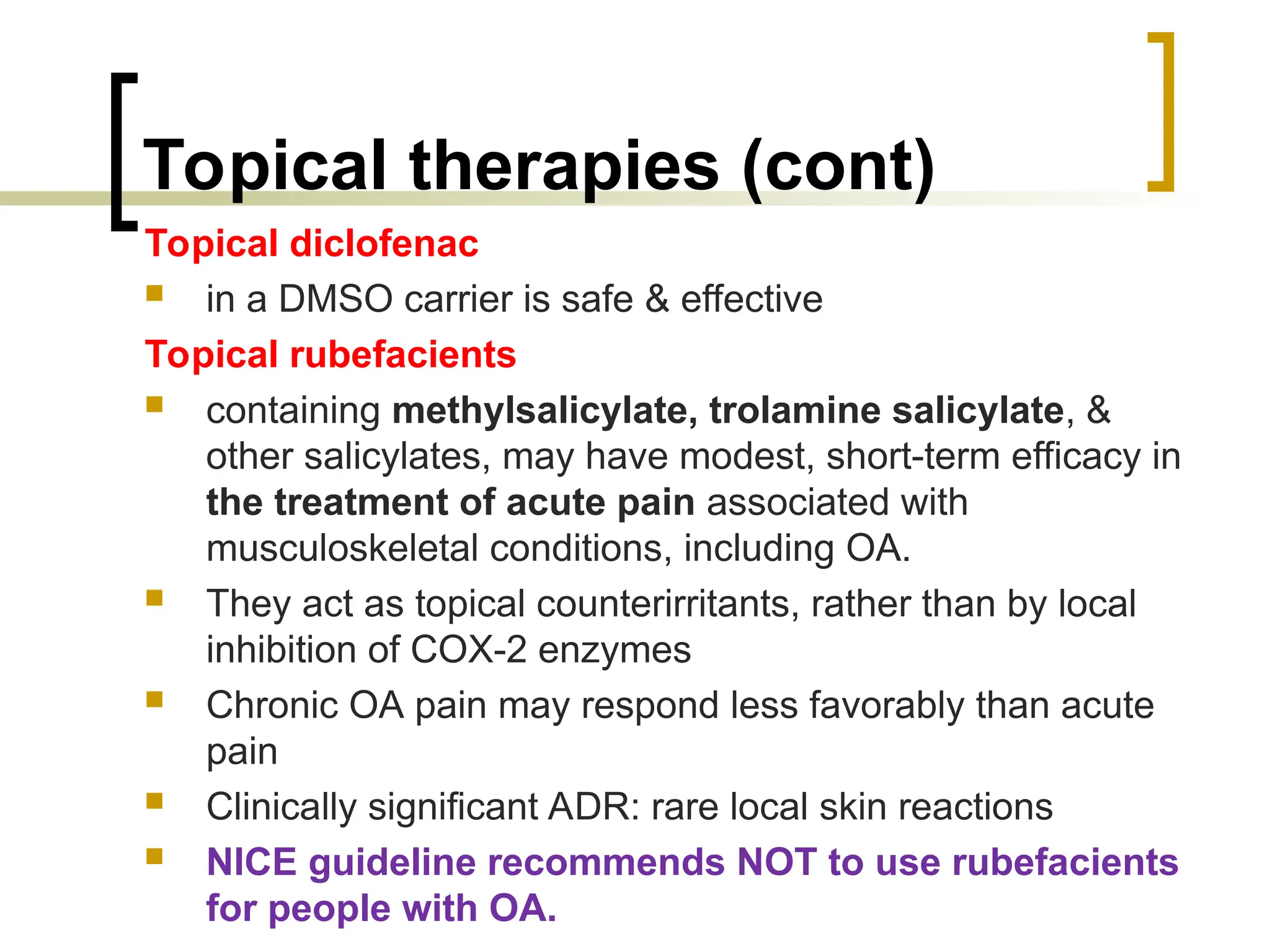
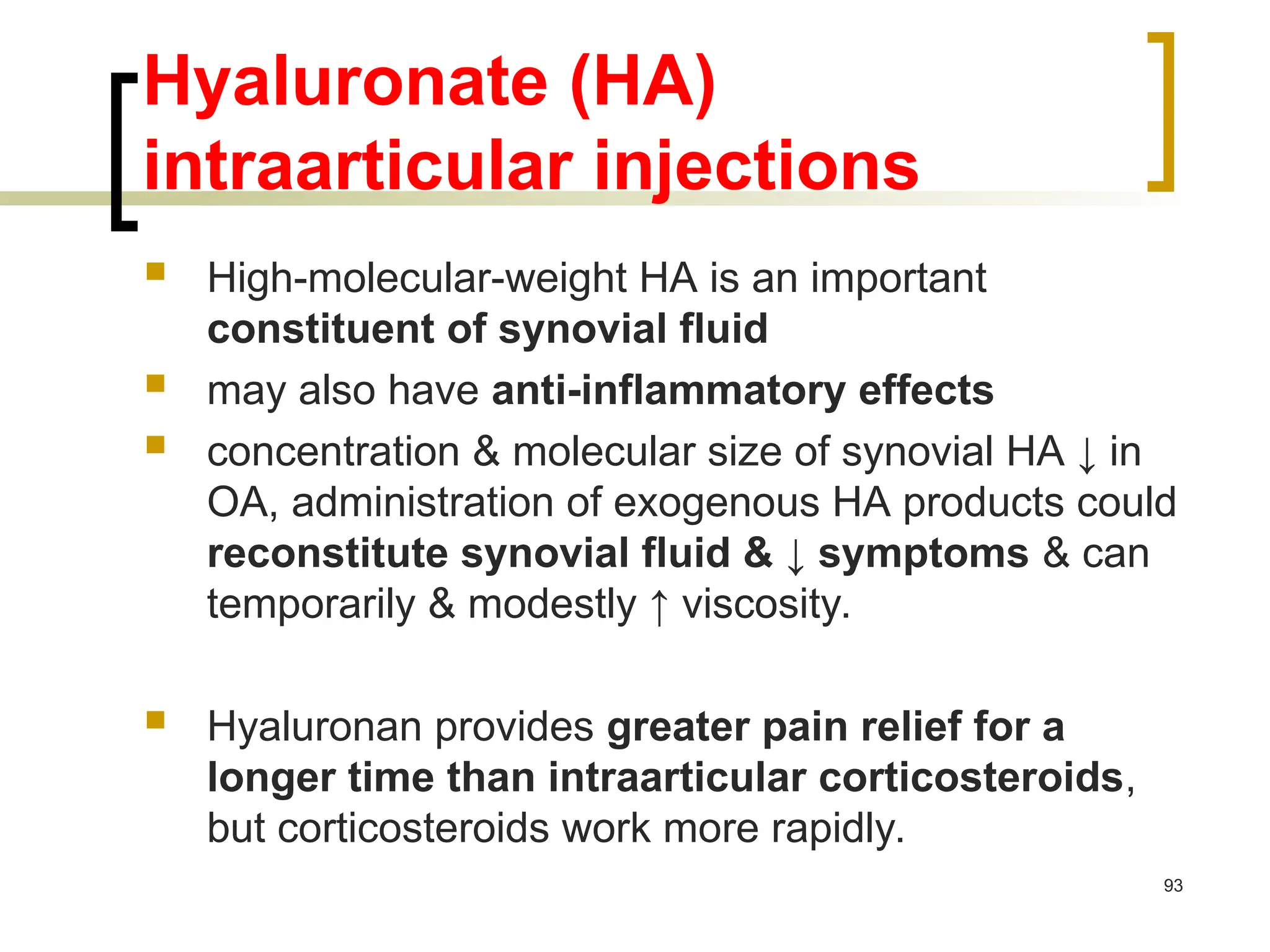
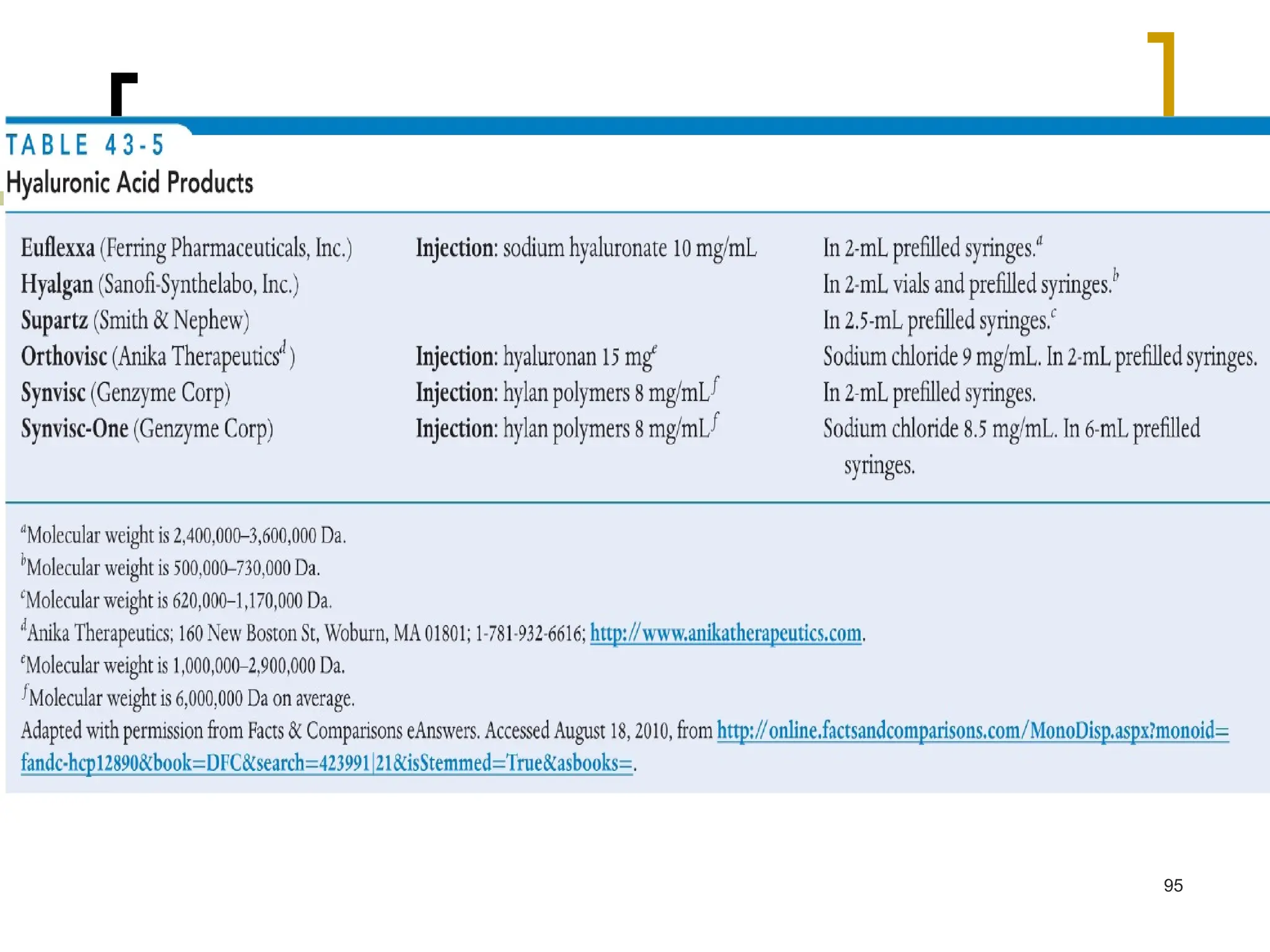
![NICE 2014 Update
Do not offer intra-articular hyaluronan
injections for the management of
osteoarthritis. [2014]
Efficacy is modest and inconsistent.
Prices of hyaluronan injections are
expensive.
94](https://image.slidesharecdn.com/6-osteoarthritis2017final-241019000400-2c281296/75/Topic-3-Osteoarthritis_2017_finalize-ppt-92-2048.jpg)