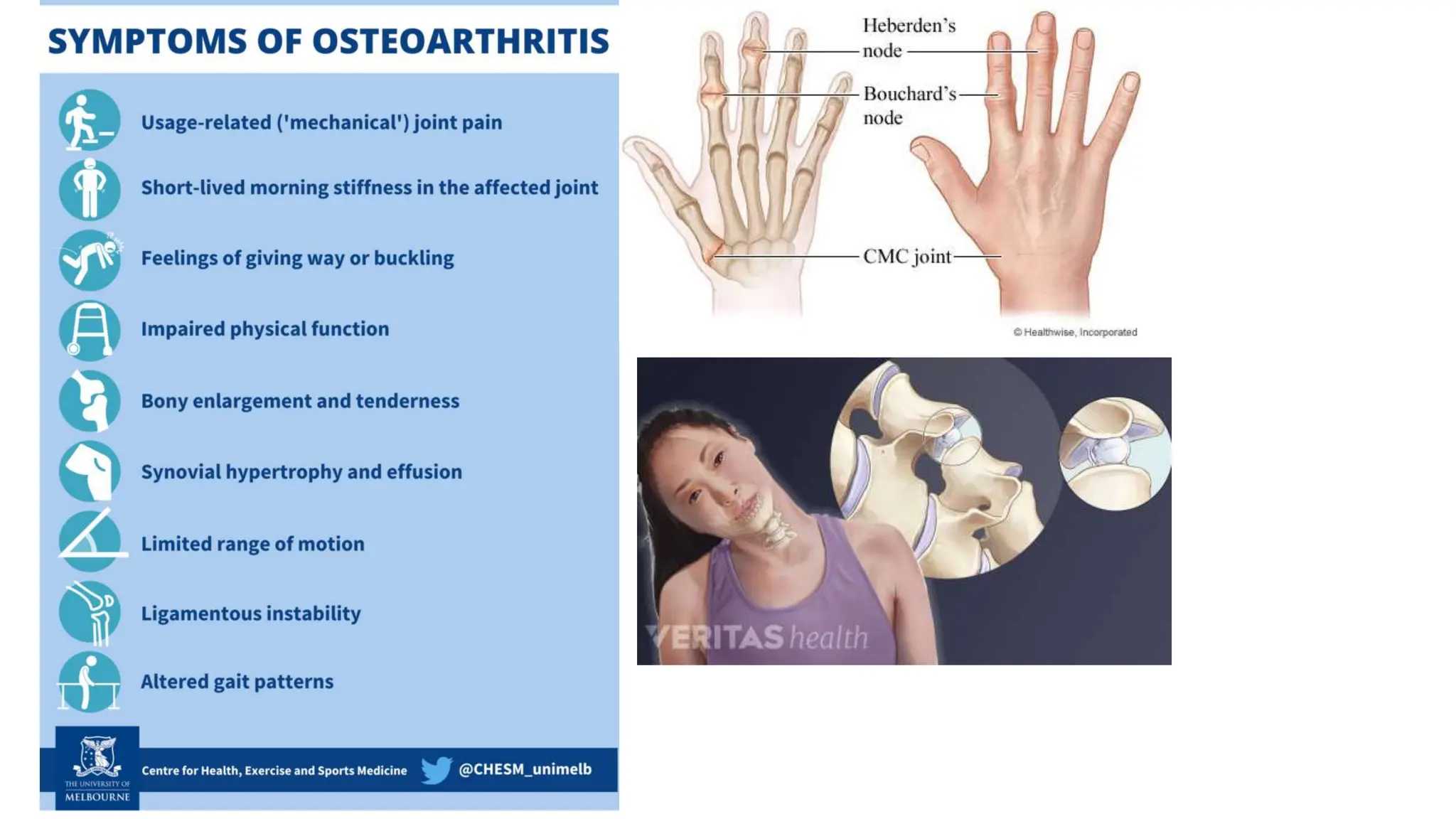
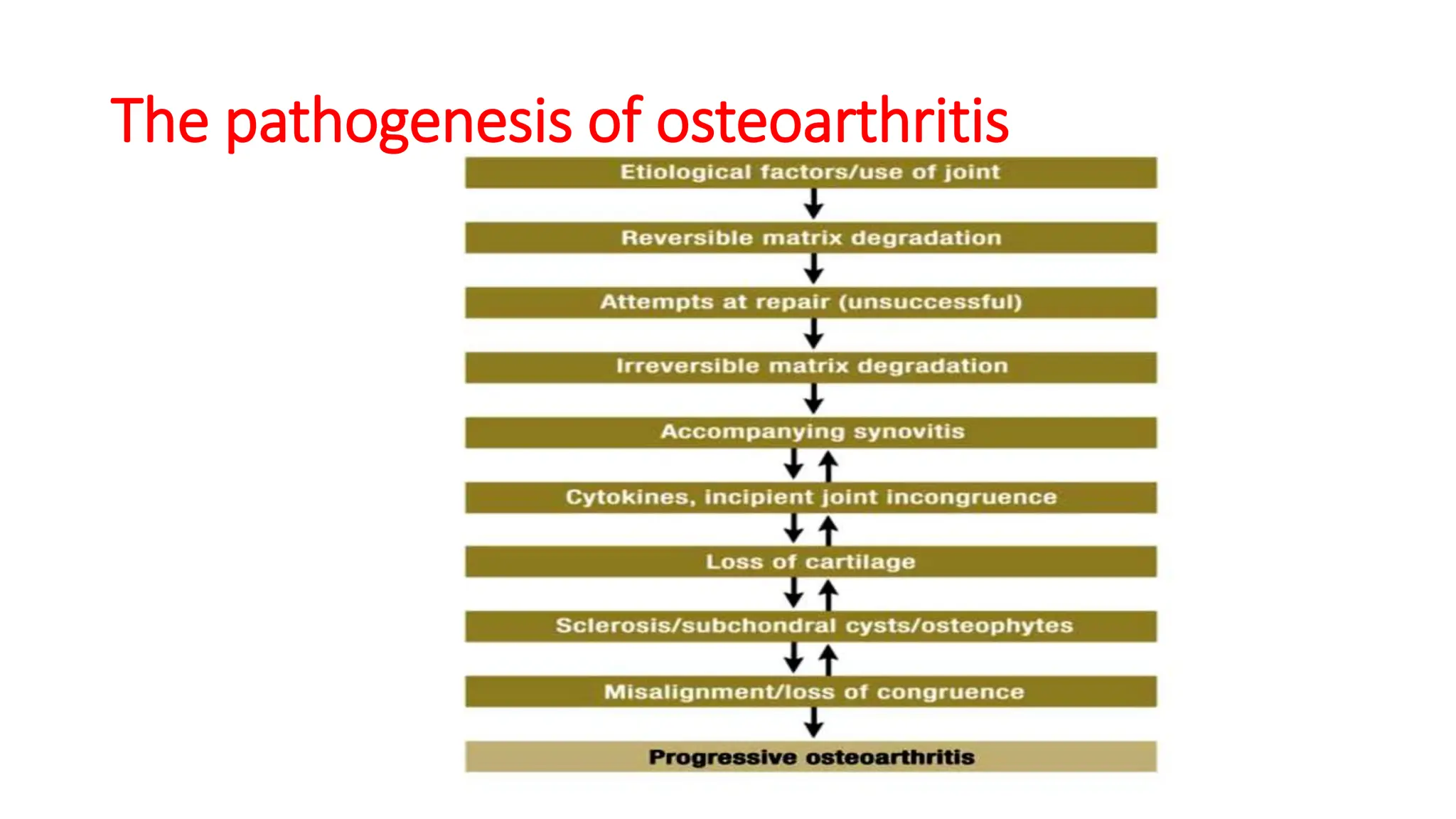
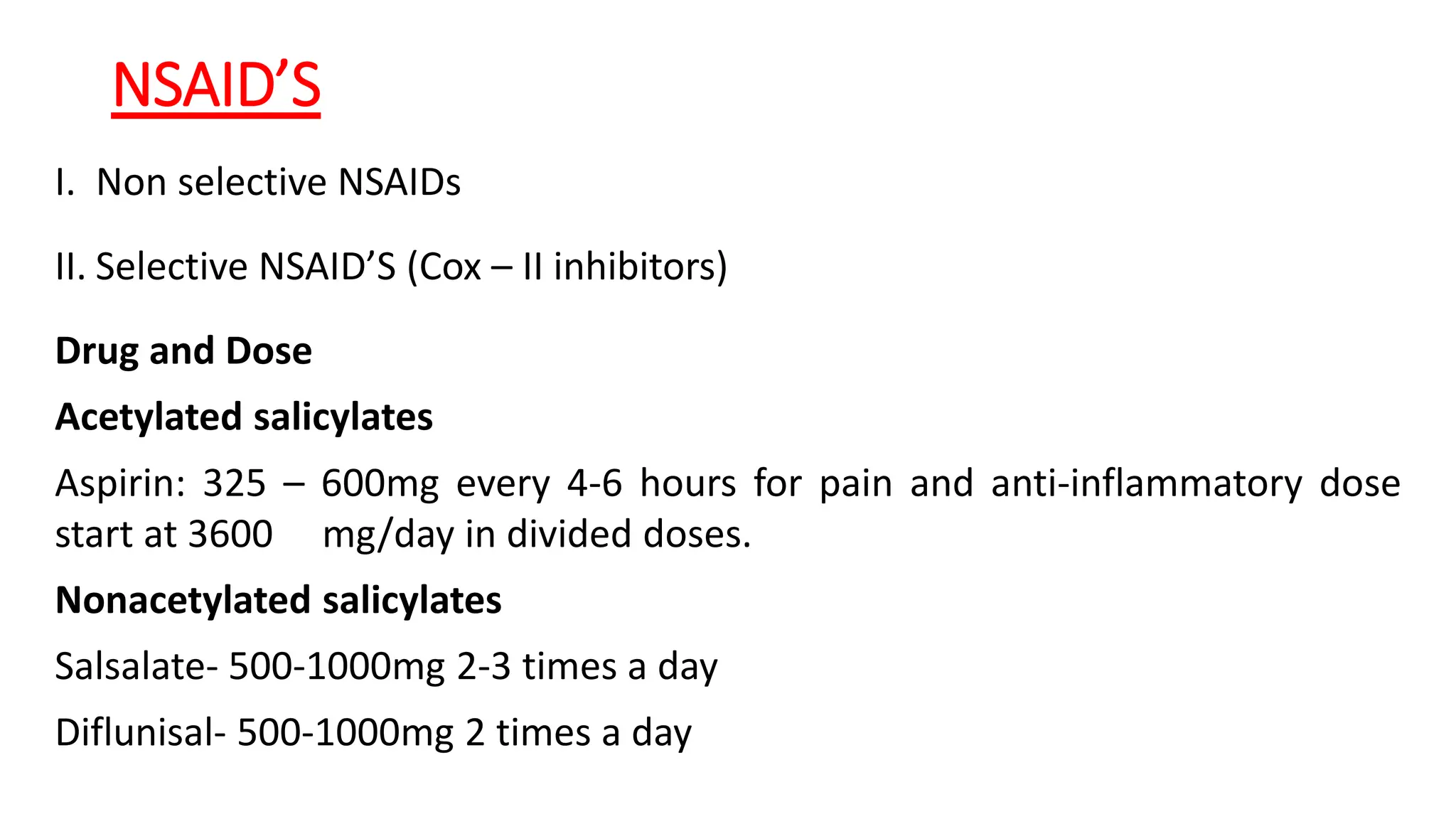
Osteoarthritis (OA) is a degenerative joint disease causing pain and disability, particularly prevalent in individuals over 50. It is characterized by the breakdown of cartilage, leading to inflammation, pain, and loss of mobility, with management focusing on pain relief, joint mobility, and improving quality of life through a combination of pharmacological and non-pharmacological therapies. Risk factors include age, joint injury, obesity, and genetic predisposition, and while OA can significantly impair daily living, there is currently no cure, only management options available.