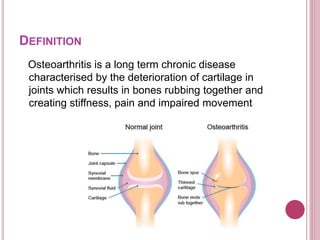
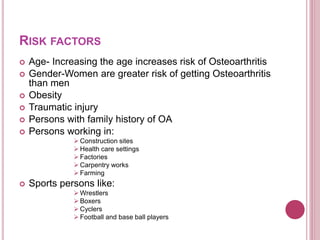
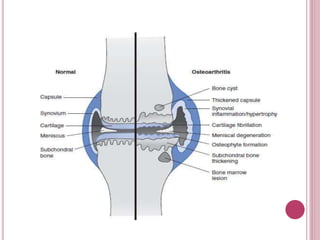
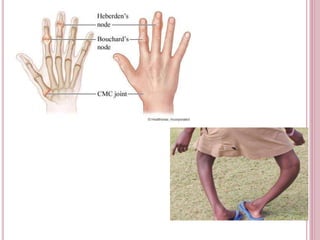
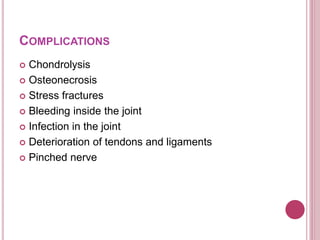
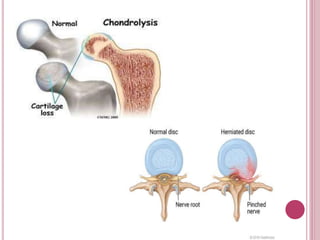
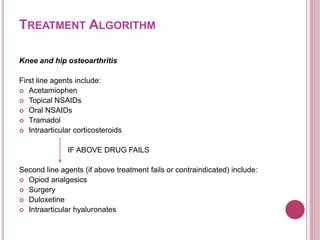
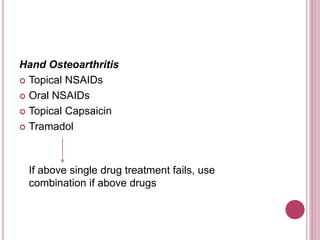
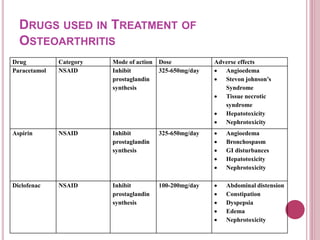
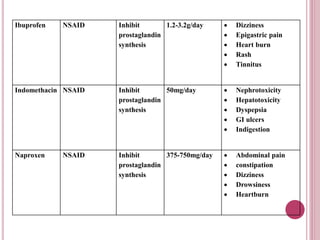
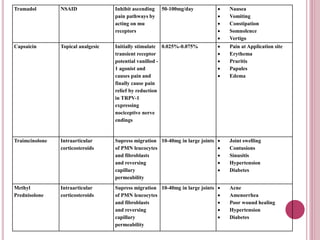
Osteoarthritis is a chronic disease characterized by the deterioration of cartilage in joints, resulting in bones rubbing together and causing stiffness, pain, and impaired movement. It is common in individuals over 60 years of age, and prevalence is higher in women than men. Risk factors include age, obesity, injury, family history, and certain occupations. Symptoms include joint pain, tenderness, and limited range of motion. Treatment involves exercise, weight loss, medications like acetaminophen, NSAIDs, and corticosteroid injections, and may require surgery like joint replacement for severe cases.