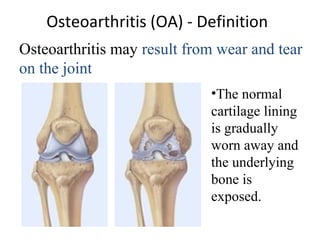
This document provides information on osteoarthritis (OA), including:
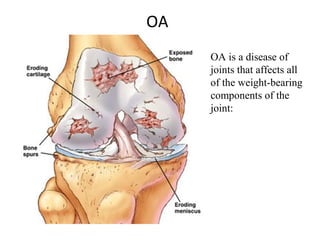
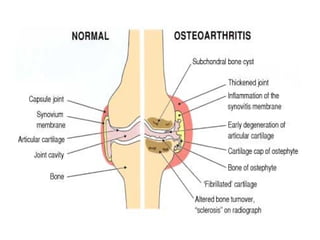
- OA is the most common form of arthritis and joint disease, typically affecting those over age 45, especially women. It commonly occurs in joints like the fingers, thumbs, neck, back, knees and hips.
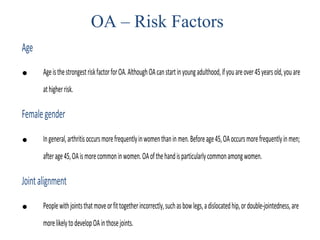
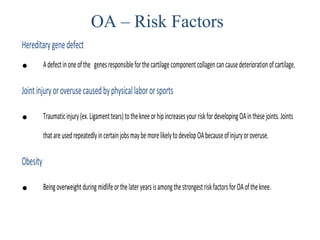
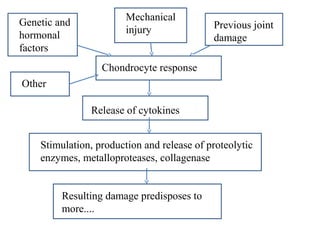
- OA can be primary (with no clear cause) or secondary (resulting from injury or other joint disease). Risk factors include age, gender, genetics, joint alignment, injury or overuse, and obesity.
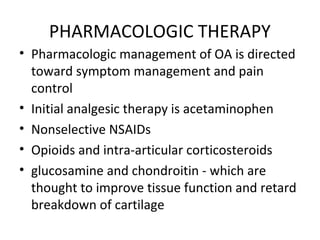
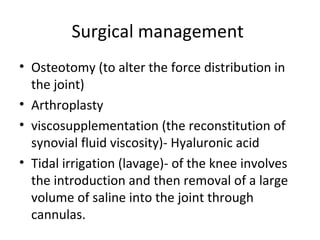
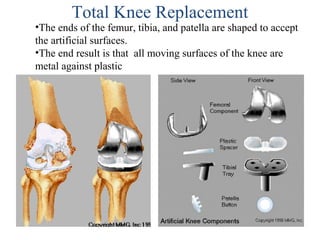
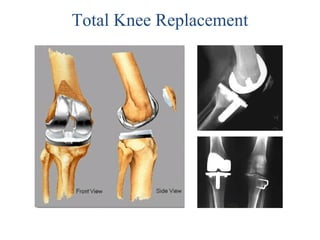
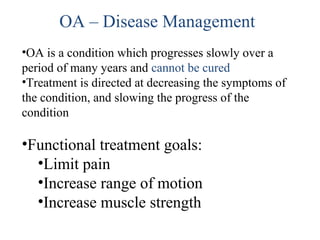
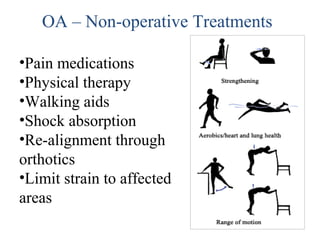
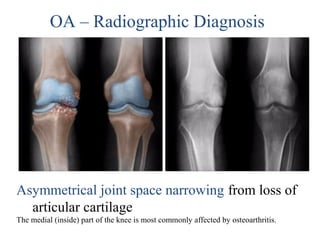
- Symptoms include joint pain, stiffness, swelling and tenderness. Diagnosis involves examining the joints and imaging tests. Treatment focuses on reducing symptoms through medications, exercise, weight loss and joint protection. Sur

![OA – Symptoms
• OA usually occurs slowly - It may be many years
before the damage to the joint becomes
noticeable
• Only a third of people whose X-rays show OA
report pain or other symptoms:
– Steady or intermittent pain in a joint
– Stiffness that tends to follow periods of inactivity, such as sleep
or sitting
– Swelling or tenderness in one or more joints [not necessarily
occurring on both sides of the body at the same time]
– Crunching feeling or sound of bone rubbing on bone (called
crepitus) when the joint is used](https://image.slidesharecdn.com/osteoarthritis-150203085644-conversion-gate01/85/Osteoarthritis-12-320.jpg)