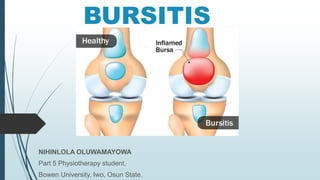
The document provides a comprehensive overview of bursitis, including its definition, causes, risk factors, clinical features, diagnosis, prevention, and treatment options. It distinguishes between true and false bursae and outlines both infective and non-infective bursitis treatments. Key topics covered include common sites for bursitis, differential diagnoses, and references for further reading.