This document provides an overview of osteoarthritis (OA), including:
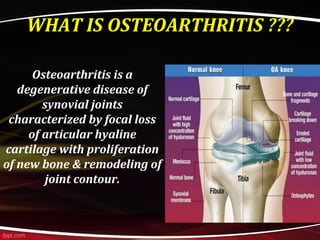
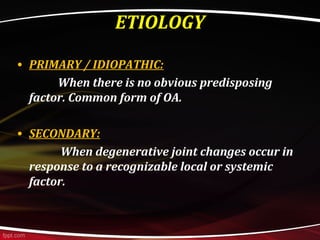
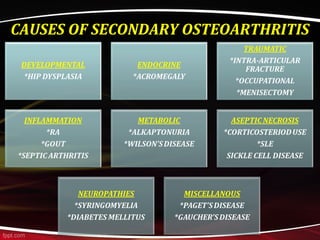
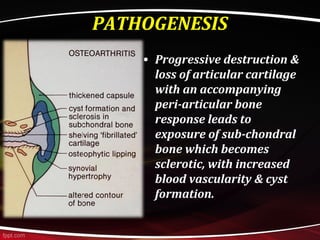
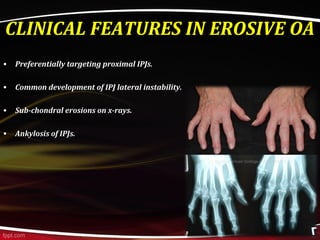
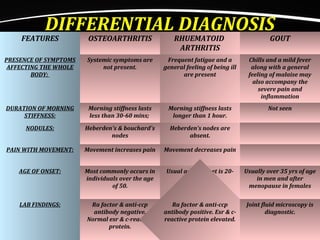
- OA is a degenerative disease affecting synovial joints, characterized by loss of cartilage and new bone growth.
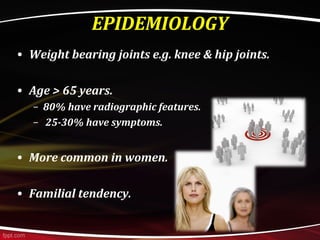
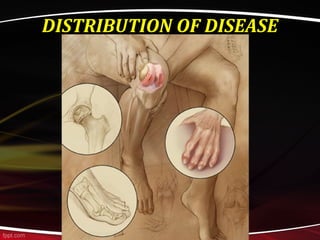
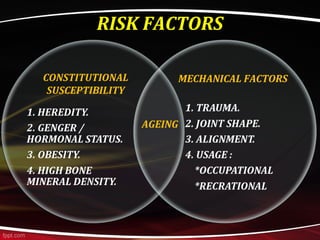
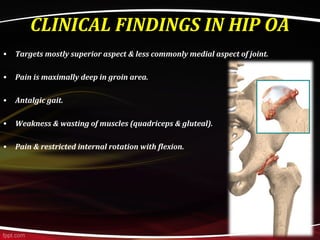
- It most commonly impacts weight-bearing joints like the knee and hip. Risk factors include age, genetics, mechanical factors.
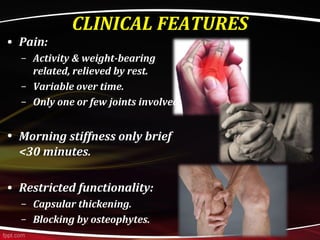
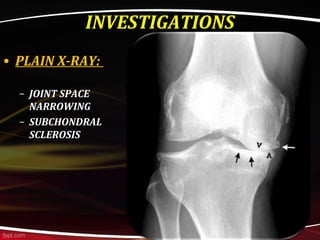
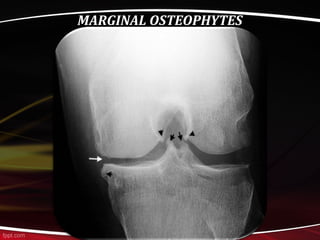
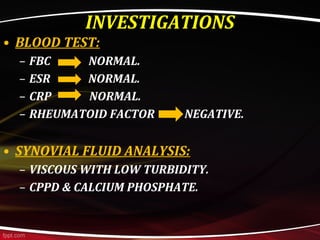
- Clinically, OA presents with pain worsened by activity that improves with rest, morning stiffness under 30 minutes, and functional limitations. Investigations include x-rays showing joint space narrowing.
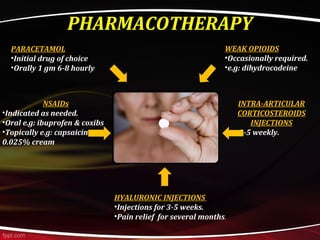
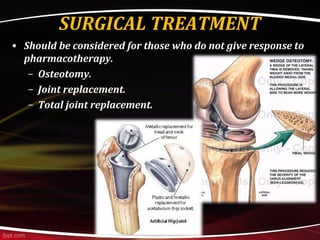
- Management involves patient education, exercises, weight loss, medications like paracetamol, NSAIDs, opioids, corticosteroid injections, hyaluronic acid injections,