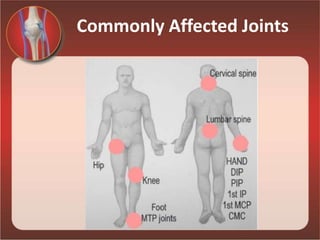
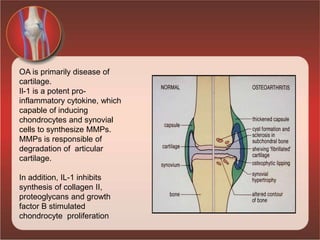
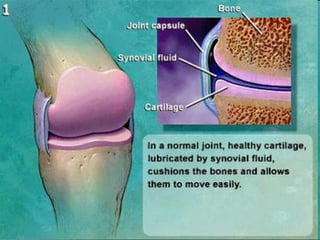
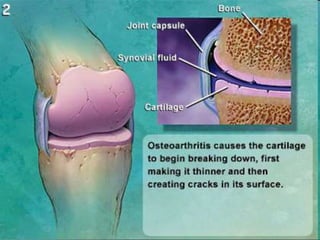
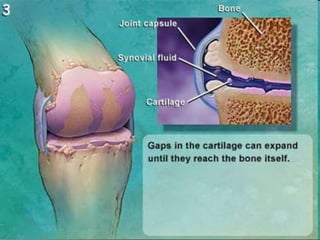
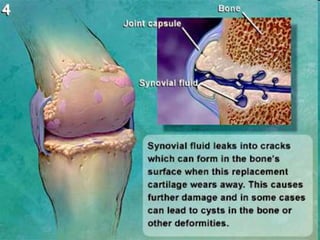
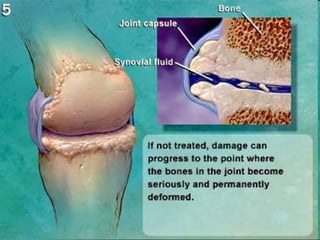
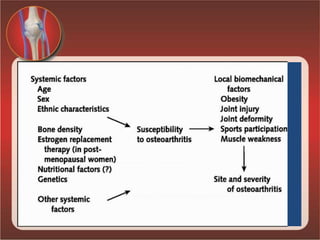
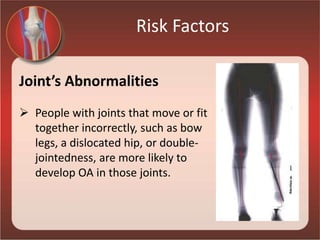
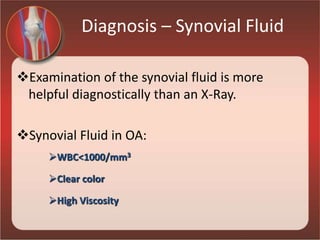
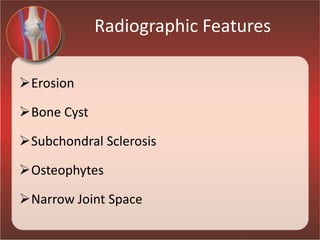
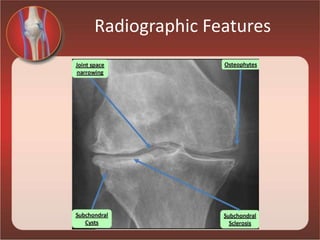
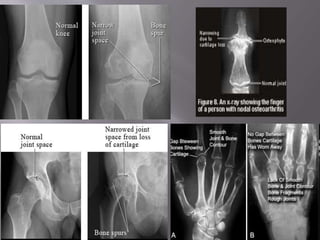
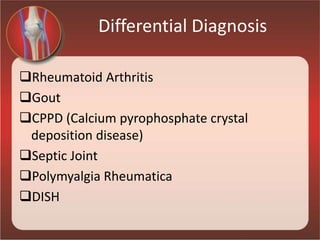
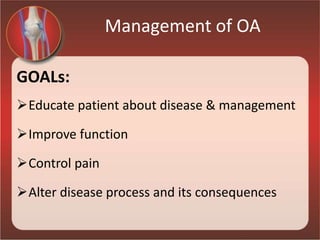
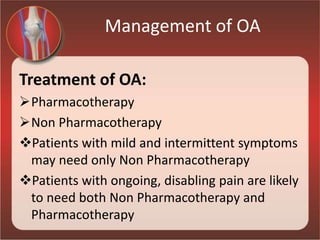
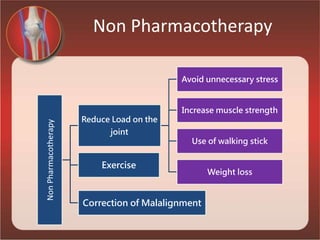
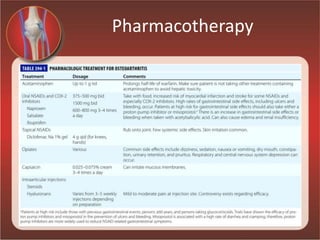
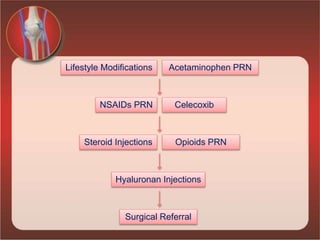
Osteoarthritis is a progressive joint disease caused by the gradual loss of cartilage. It is the most common form of arthritis and joint disease. The commonly affected joints are those in the hands, feet, spine, and knees. Risk factors include age, female gender, genetics, obesity, joint injuries, and overuse. Symptoms include joint pain, stiffness, and loss of function. Diagnosis involves physical exam, x-rays showing bone spurs and joint space narrowing, and ruling out other arthritic conditions. Treatment focuses on reducing joint stress through exercise, weight loss, and assistive devices. Medications may include acetaminophen, NSAIDs, and opioids for pain. Injections and surgery are