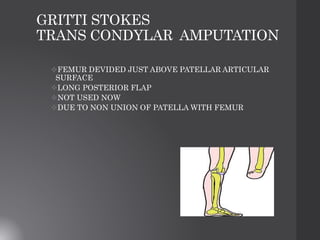
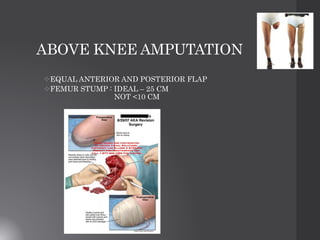
This document provides information about amputation procedures. It describes the indications for amputation, including peripheral vascular disease, diabetic limb disease, trauma, infection, malignancy, and deformity. The goals of amputation are to return the patient to maximum function, ablate diseased tissue, reduce morbidity and mortality, and produce a physiological end organ. Different types of amputations are described for the toes, feet, legs, arms, and limbs. Principles for determining the amputation level and performing the procedure are outlined. Postoperative management focuses on wound healing, edema control, pain management, and rehabilitation to prevent contractures. Potential complications are also reviewed.