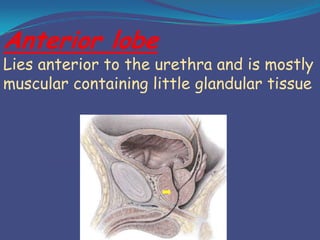
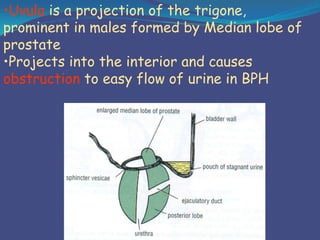
This document provides an overview of the anatomy and surgical procedures related to the prostate gland. It begins with the surgical anatomy of the prostate, including its relations to surrounding structures, coverings, lobes, blood supply, lymphatic drainage and innervation. It then discusses various prostate surgeries like TURP, open and laparoscopic prostatectomy. It concludes with potential complications of prostate surgery, such as injuries, urinary incontinence, and issues with erection, ejaculation and fertility. Videos are also embedded to demonstrate different prostate procedures.