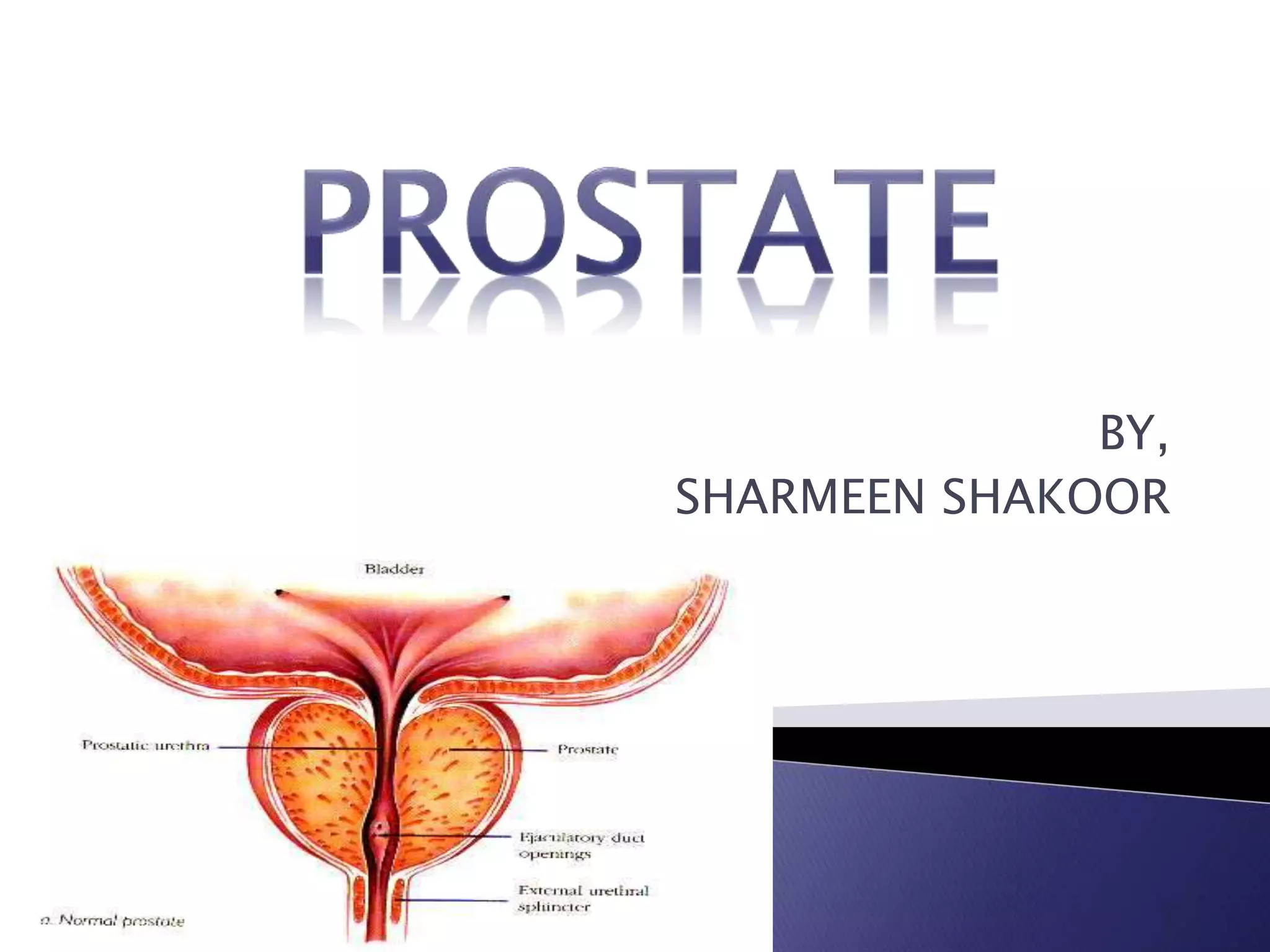
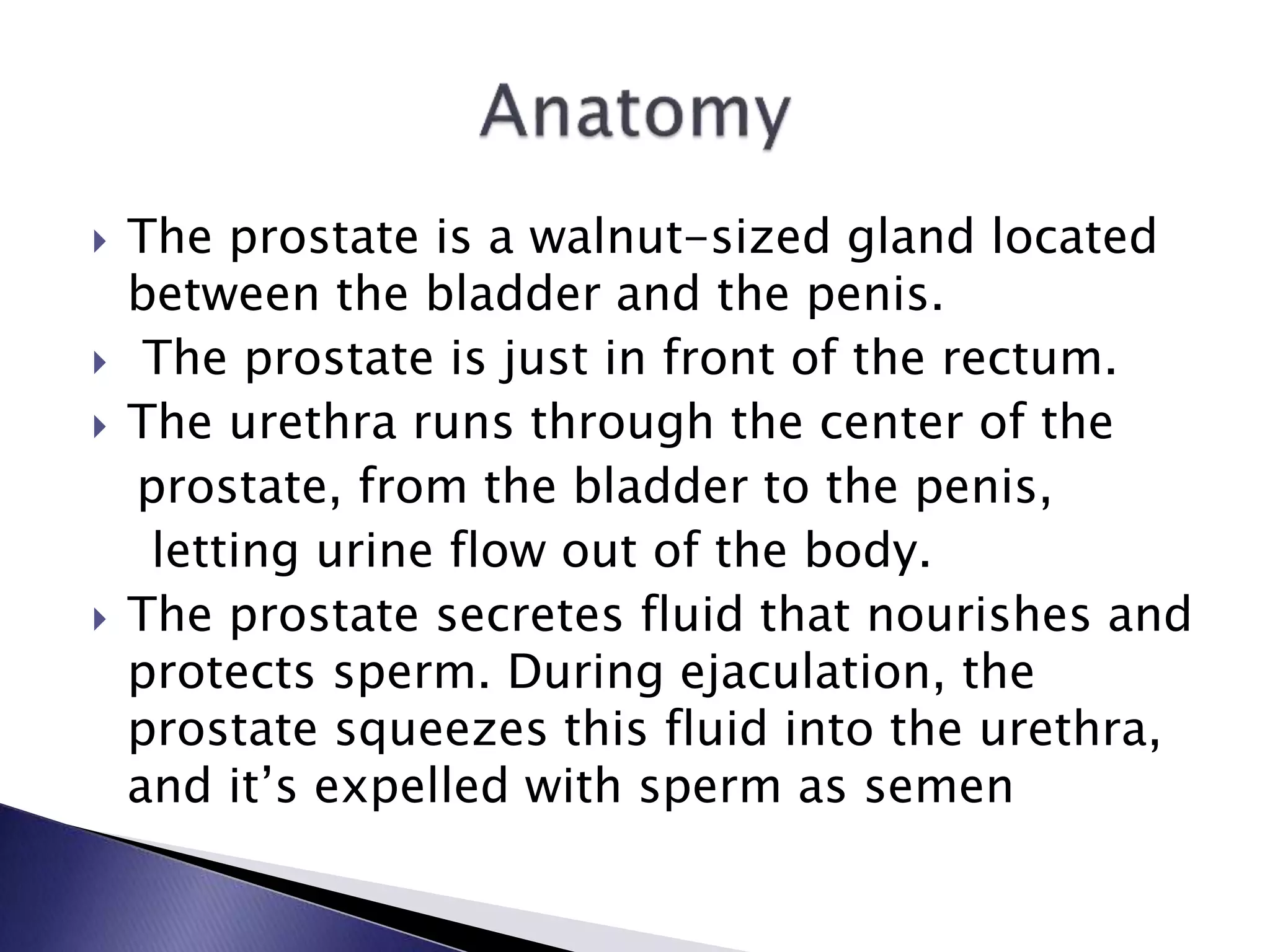
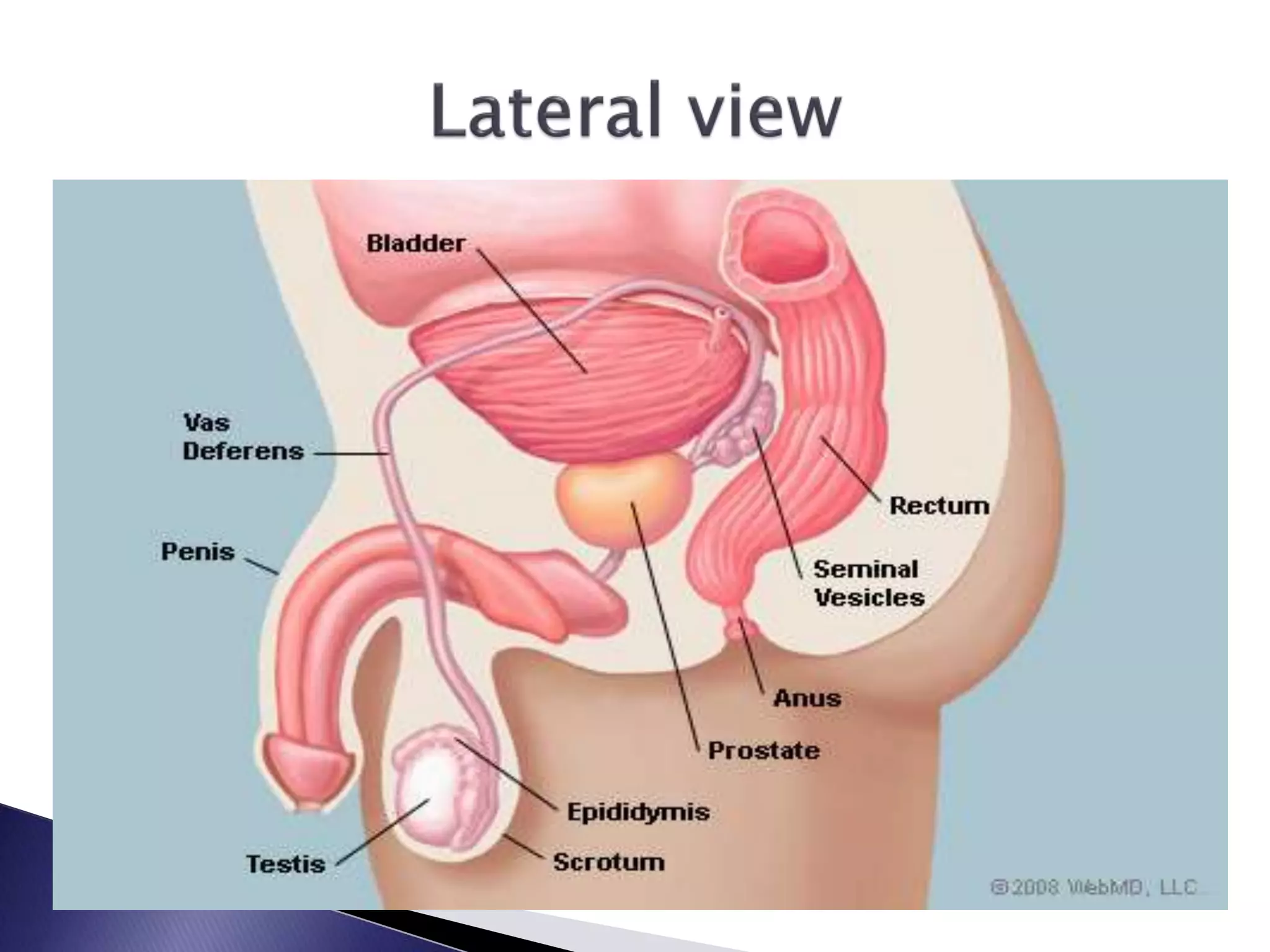
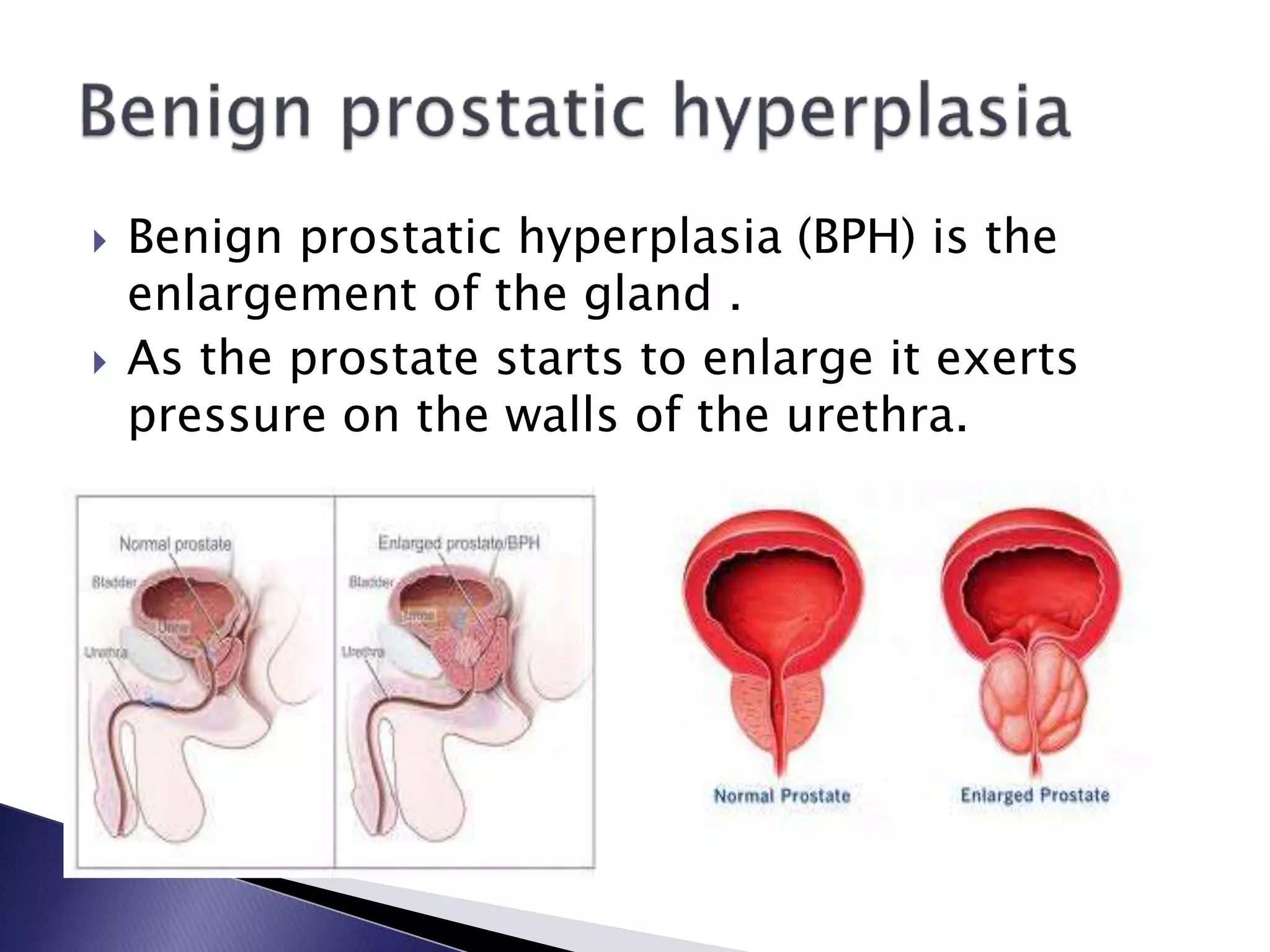
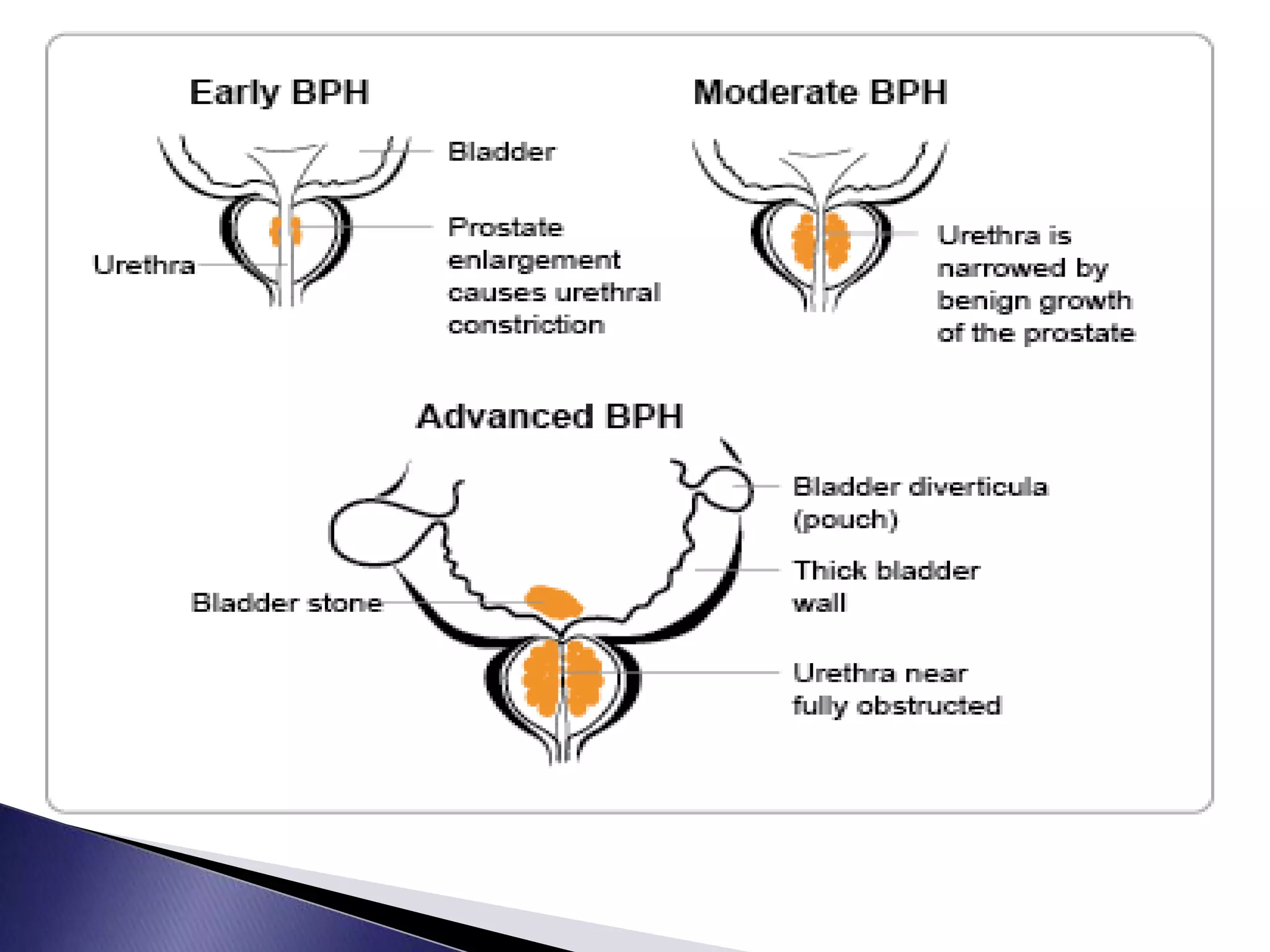
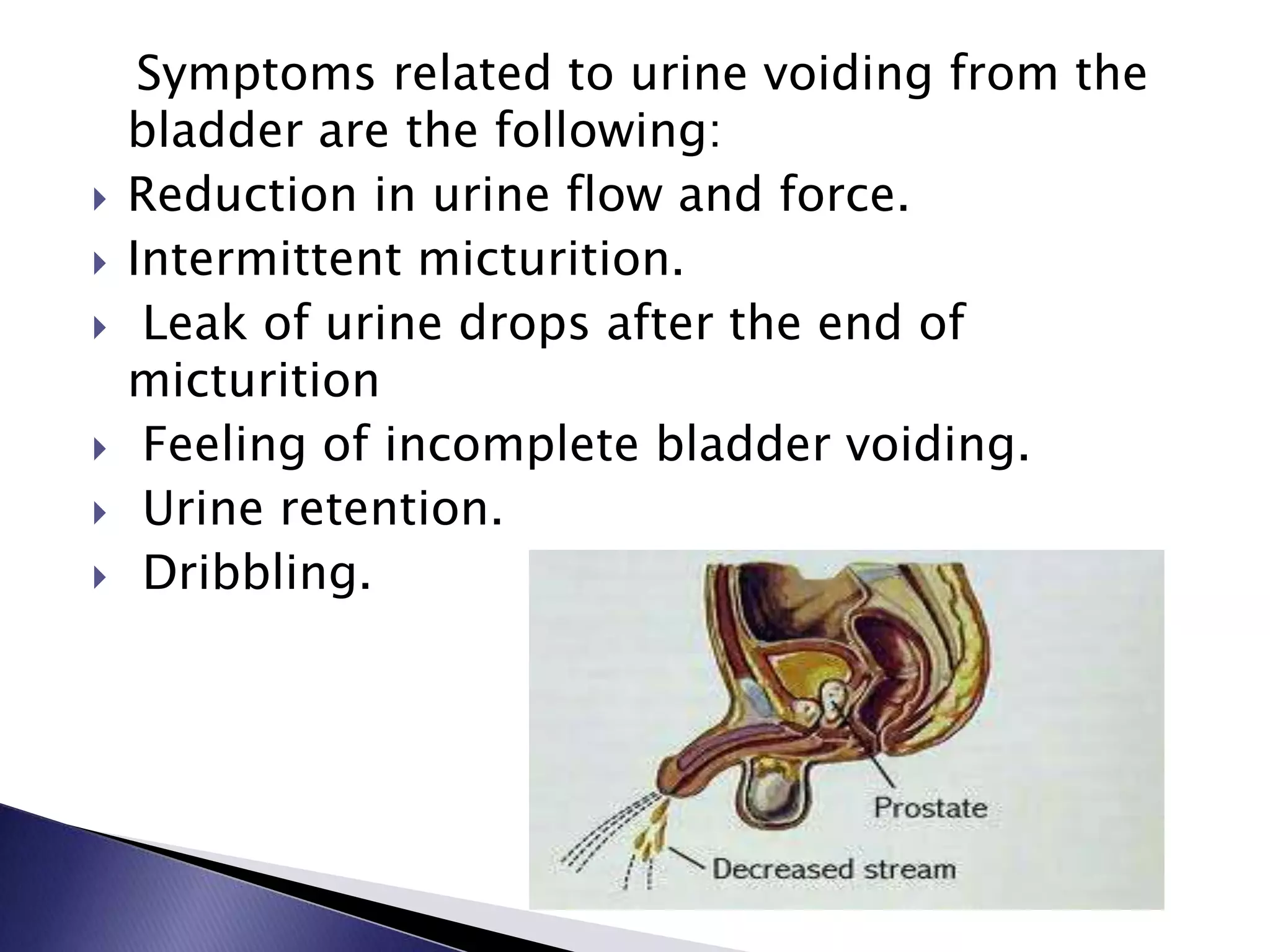
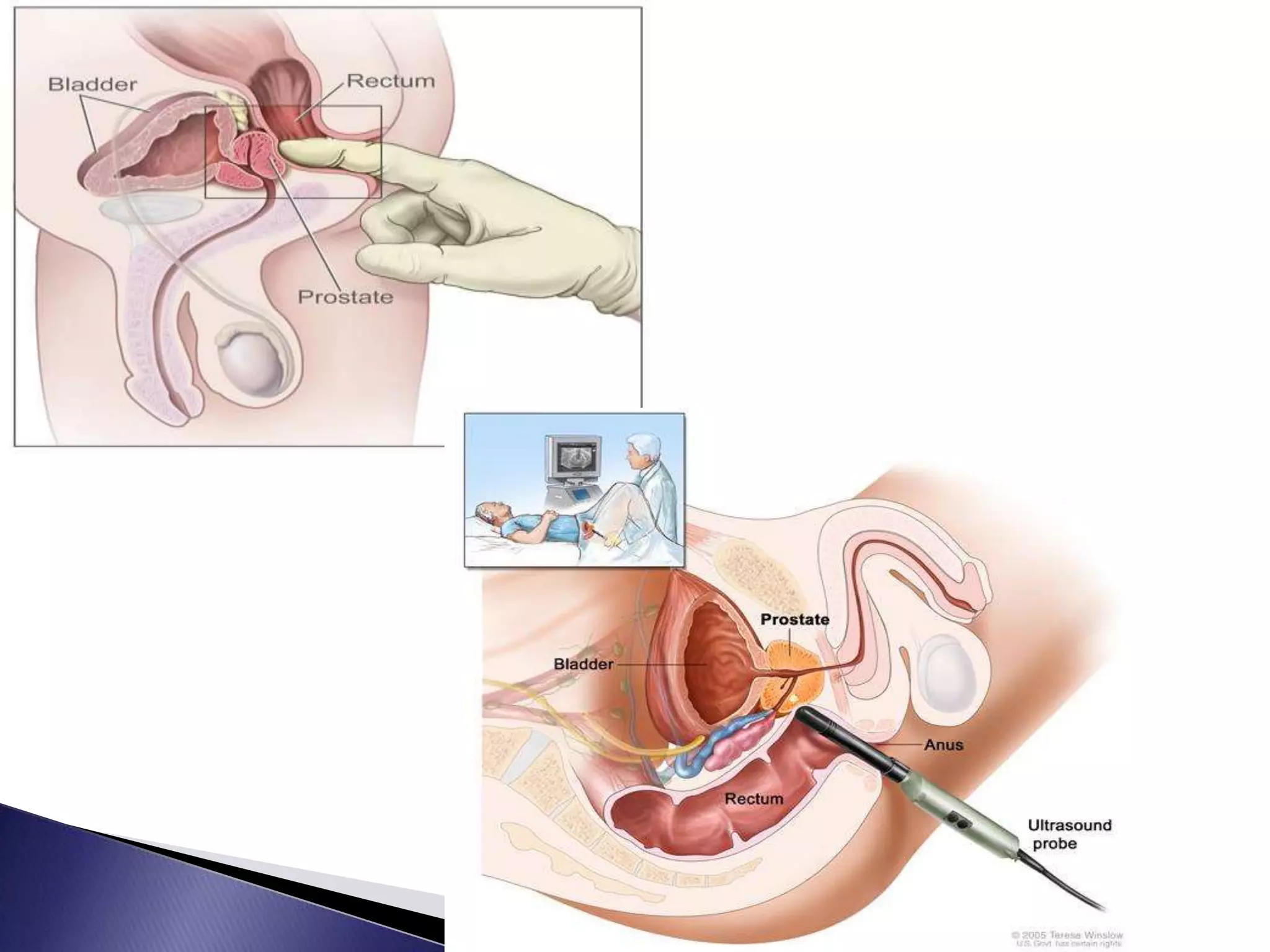
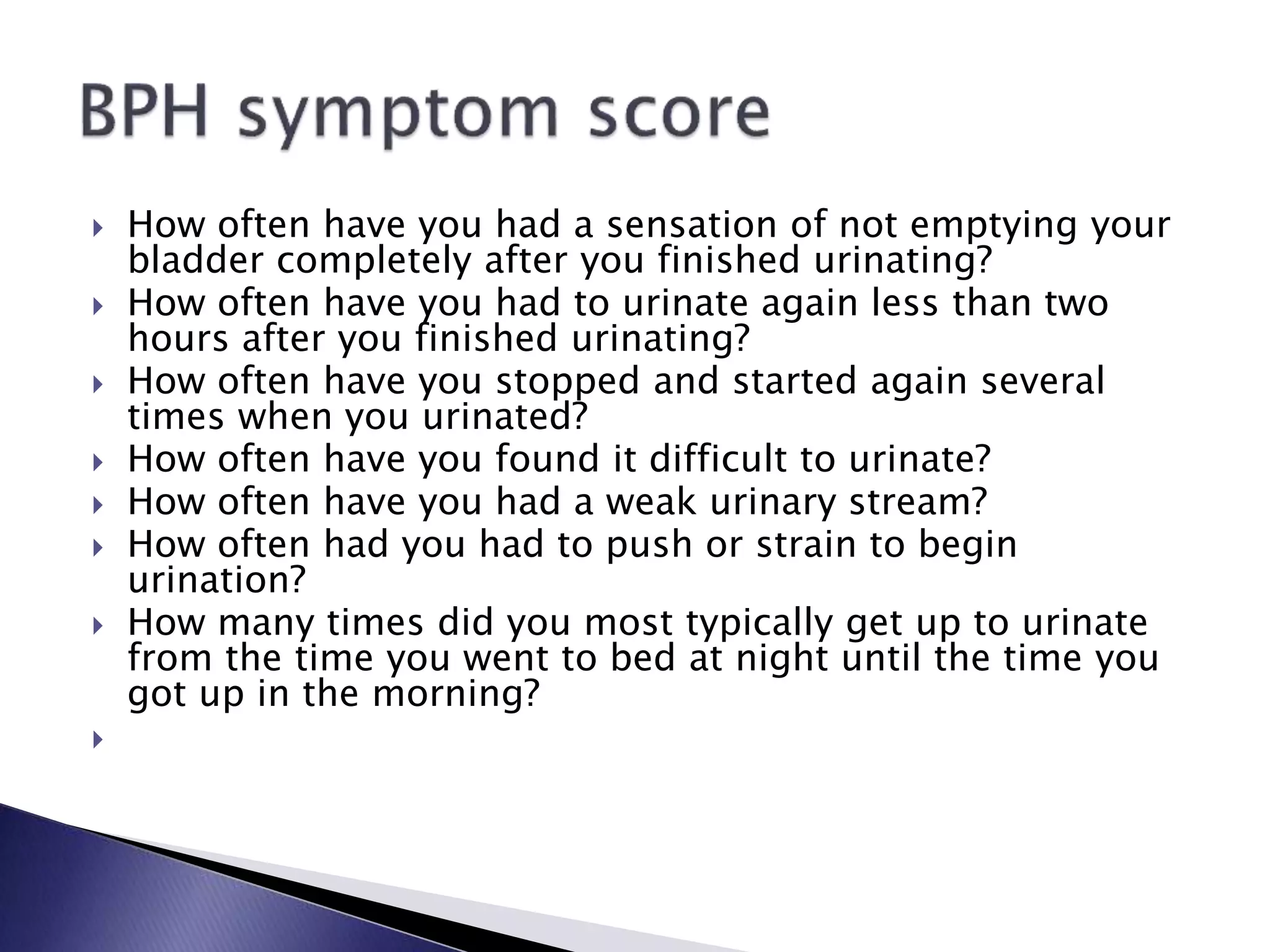
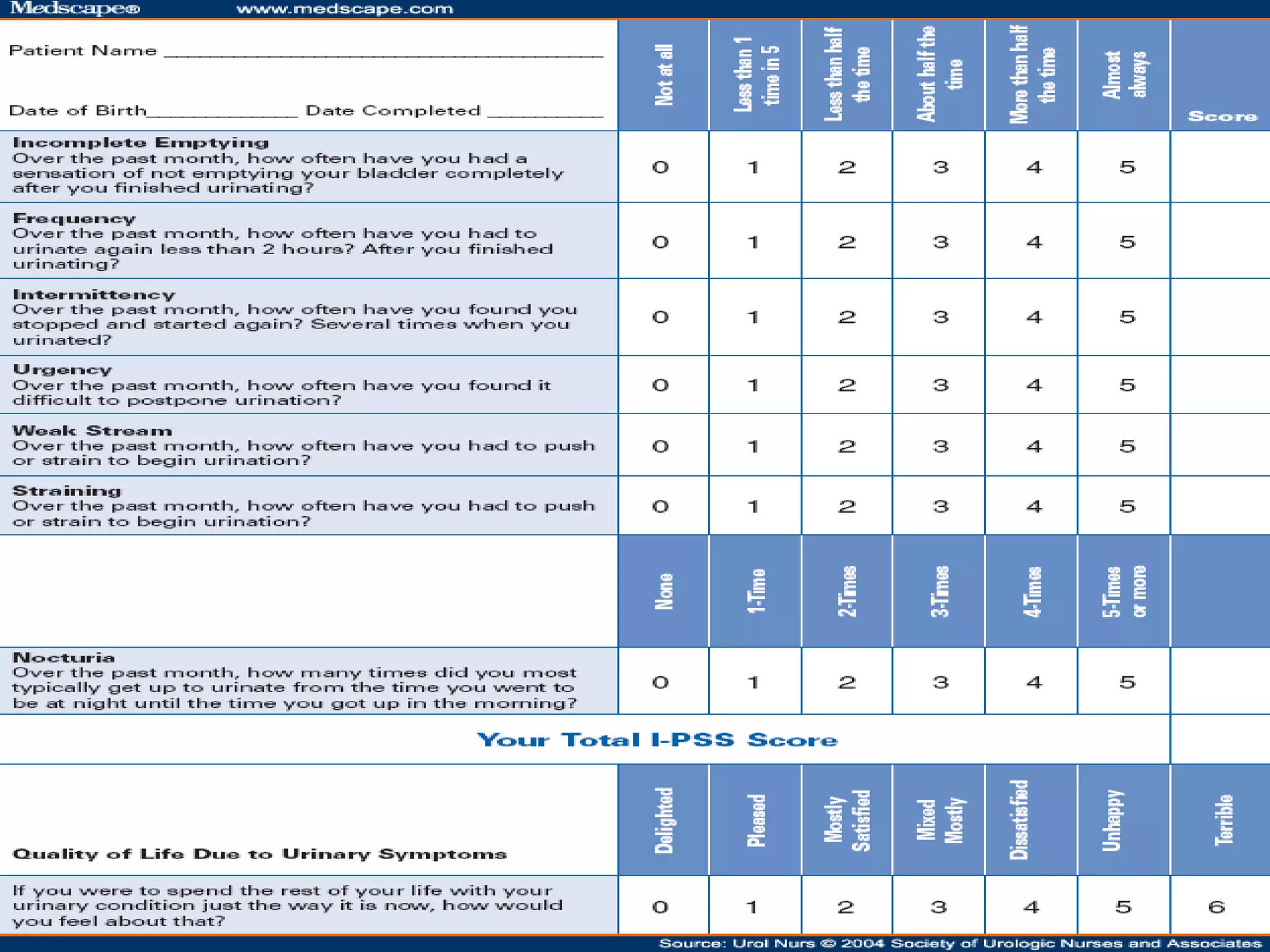
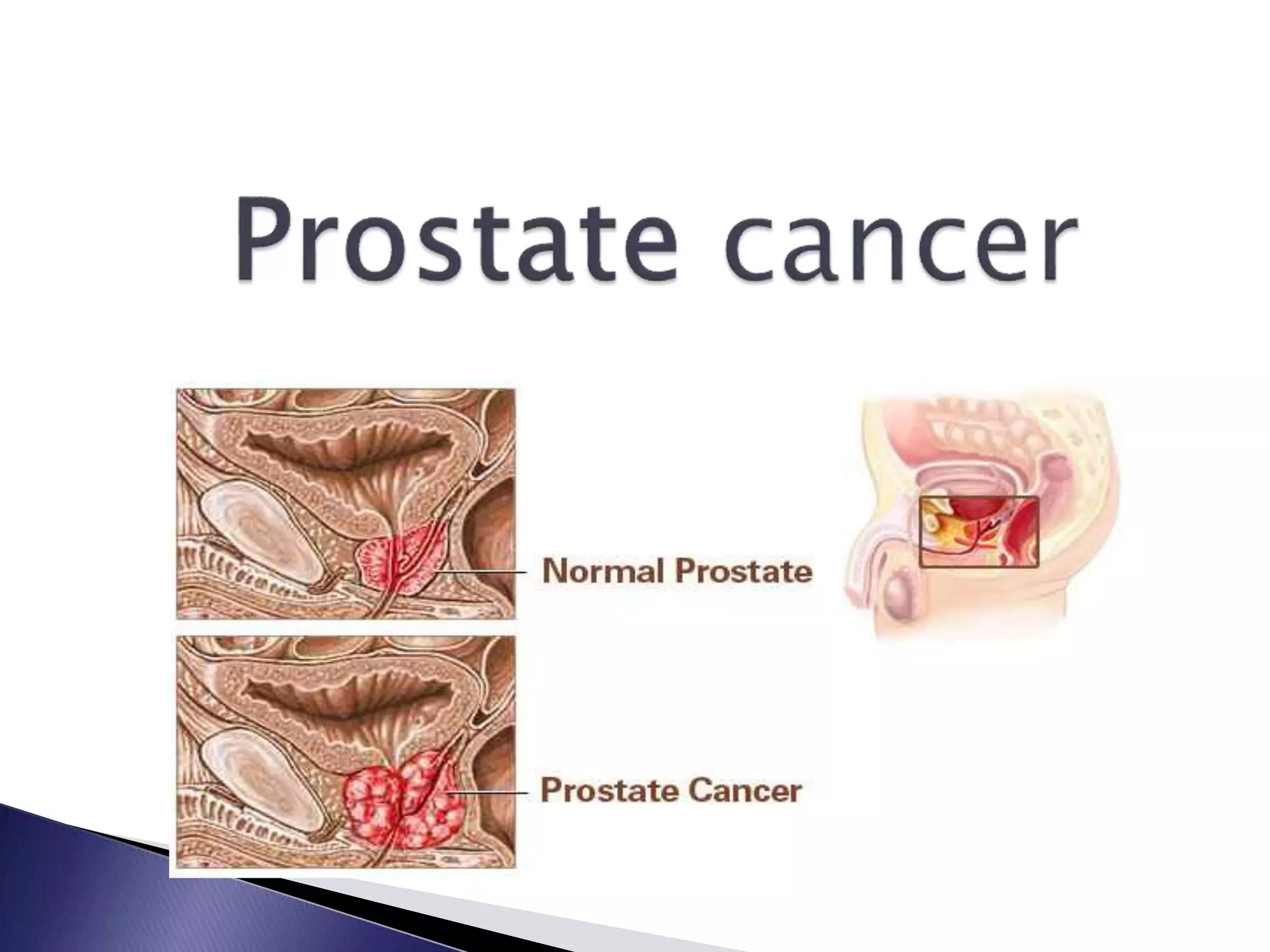
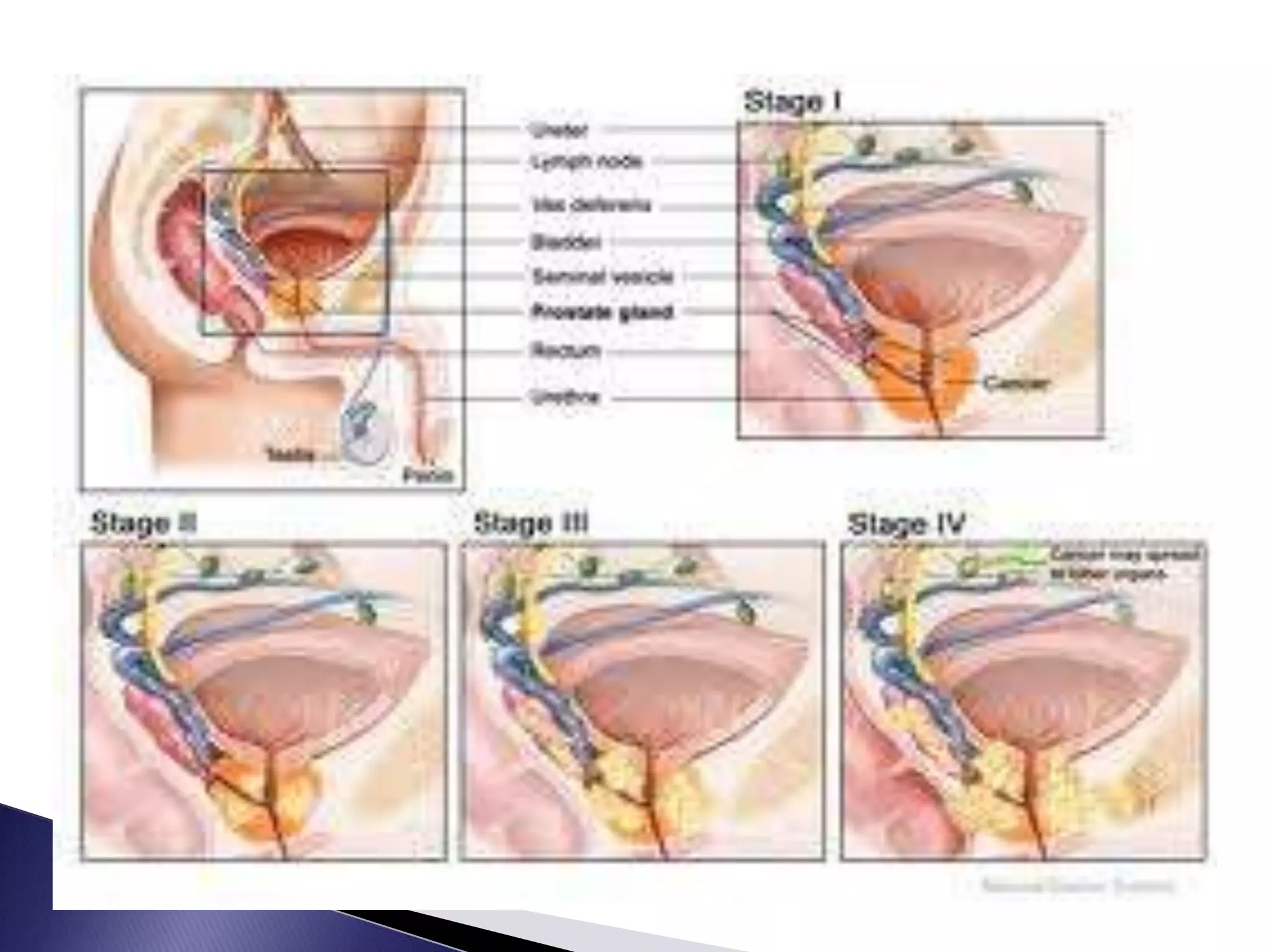
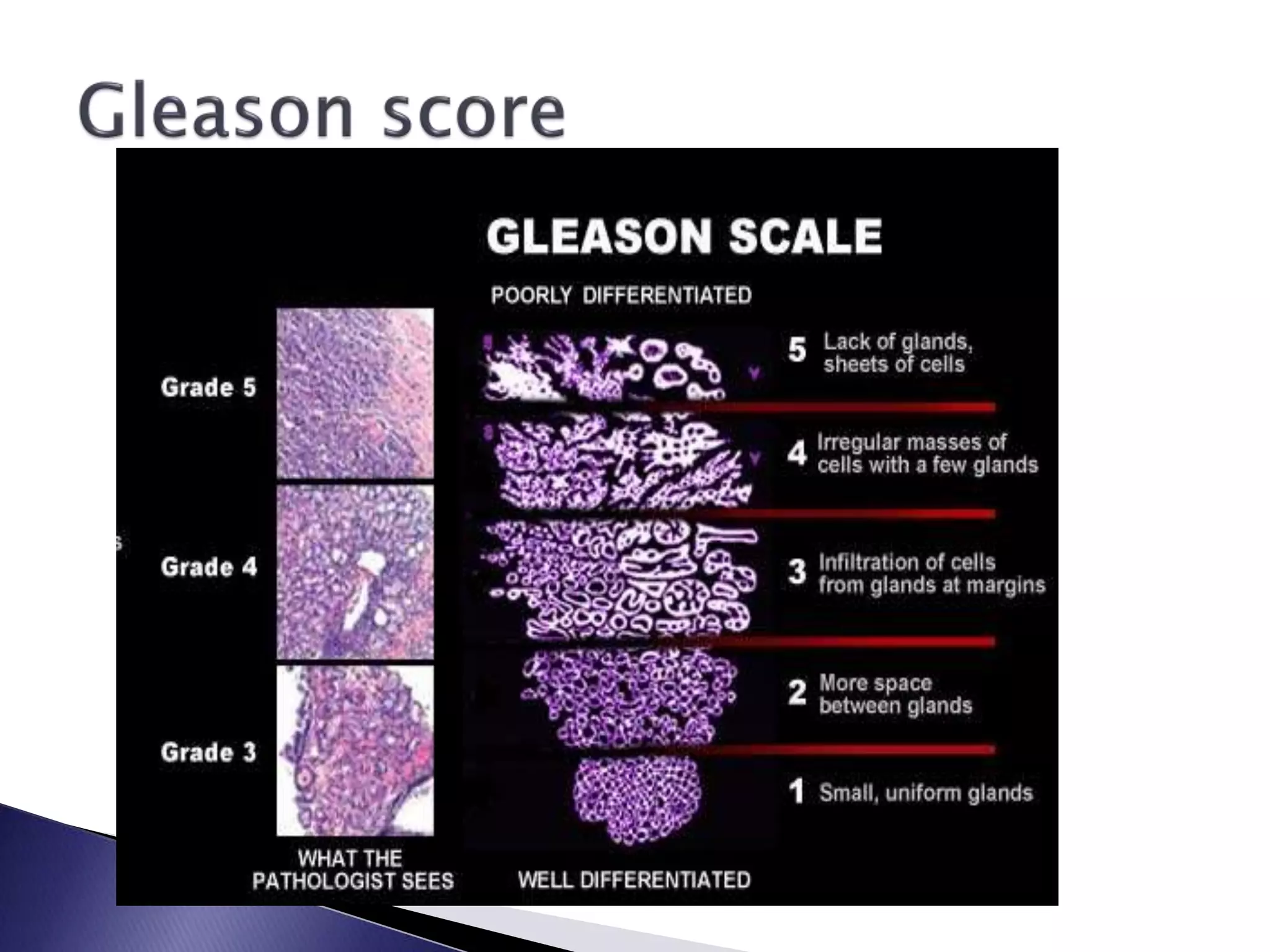
The document discusses the anatomy and functions of the prostate gland. It is located below the bladder and in front of the rectum. The prostate secretes fluid that nourishes sperm. Common prostate problems include enlarged prostate (BPH), prostate cancer, and prostatitis. BPH causes urinary symptoms due to pressure on the urethra. Prostate cancer develops from gland cells and can spread to other organs if not detected early. Diagnosis involves exams, tests like PSA, and biopsies. Treatment depends on the condition but may include medications, surgery, radiation, or watchful waiting.