This document provides tips for using a PowerPoint presentation on anatomy. It recommends:
- Freely editing and modifying the slides
- Showing blank slides first to elicit student responses before presenting content
- Repeating this process of blank slides followed by content slides three times for active learning
- Using the presentation also for self-study
- Checking the notes for bibliographic references
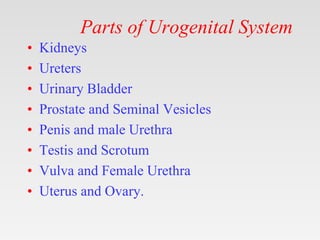
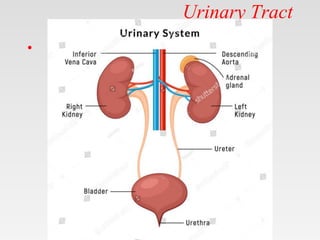
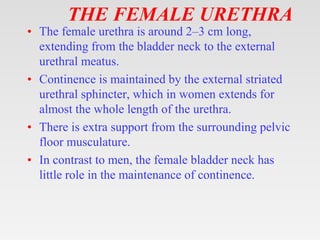
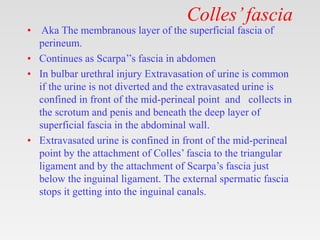
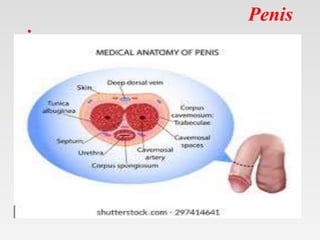
It then provides an outline of slides on the urogenital system and its parts, with detailed slides on anatomy of the kidneys, ureters, bladder, and male and female urethra.