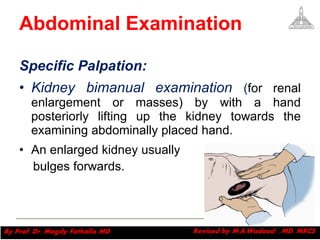
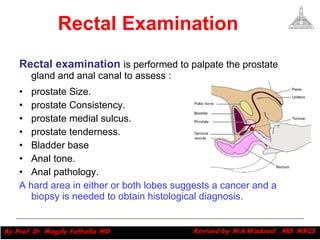
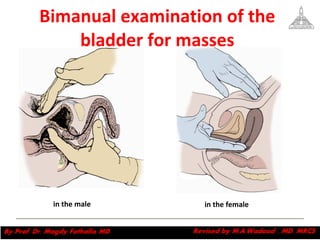
Urological symptoms can involve pain, changes to urination, changes in urine appearance, or abnormalities of the male genitalia. A complete history divides into chief complaint, history of present illness, past medical history, family history, and review of systems. Physical exam includes inspection and palpation of the abdomen with specific examination of the kidneys, bladder, and genitalia. Common urological complaints involve sites of pain, irritative urinary symptoms, obstructive symptoms, incontinence, hematuria, and sexual or genital abnormalities.