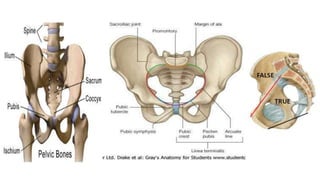
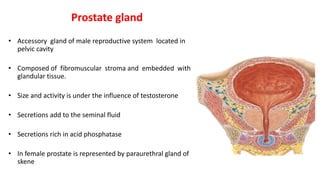
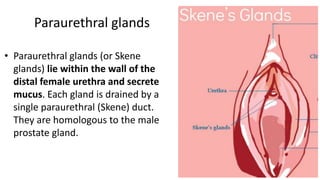
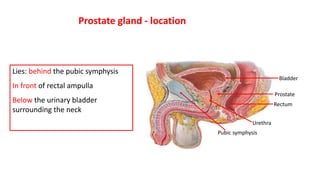
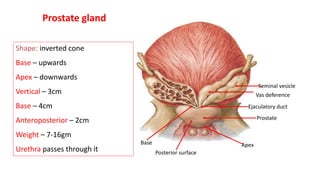
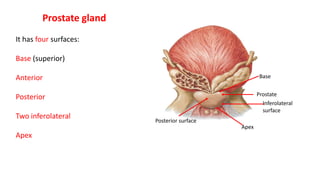
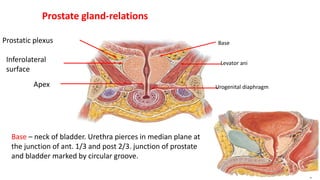
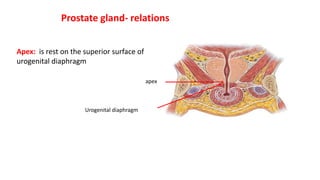
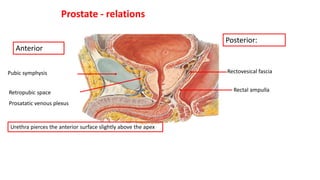
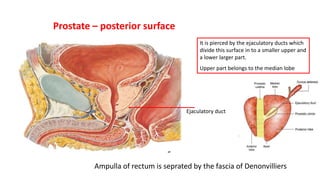
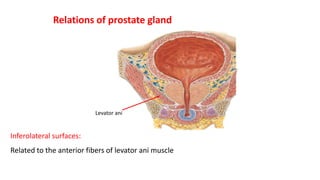
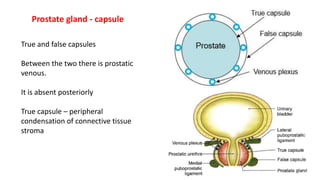
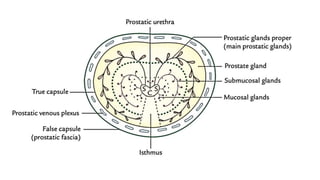
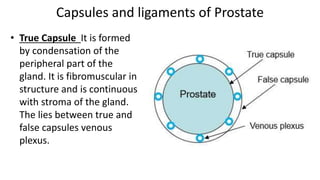
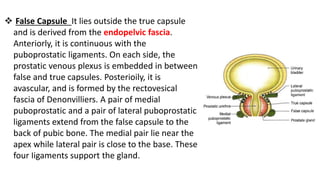
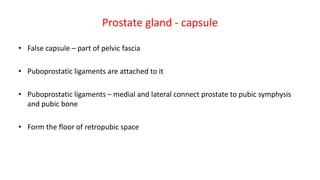
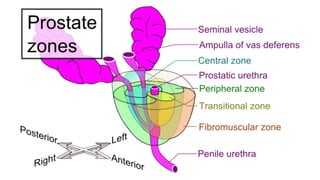
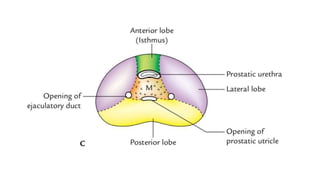
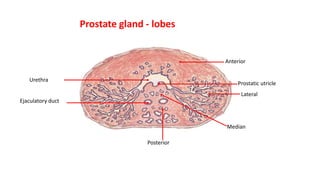
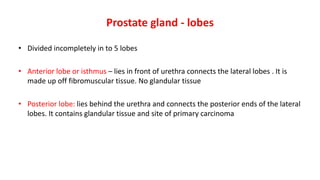
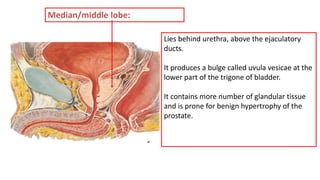
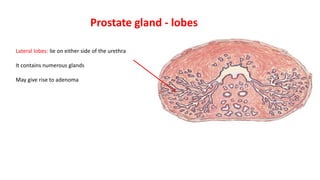
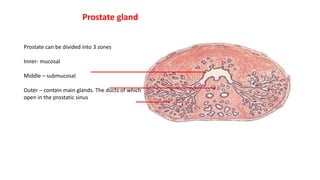
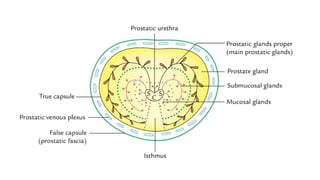
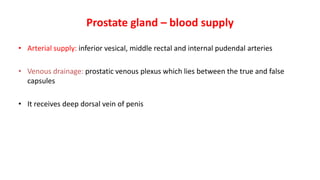
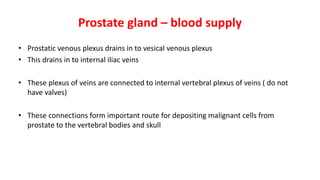
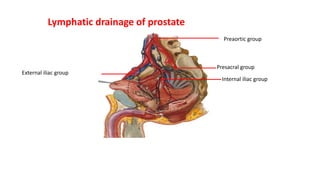
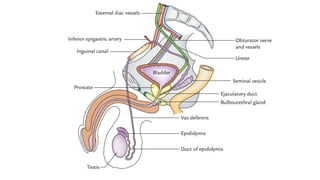
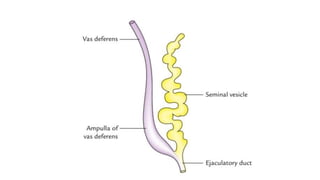
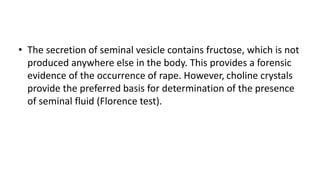
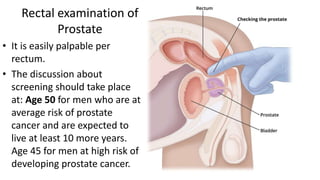
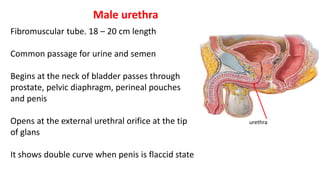
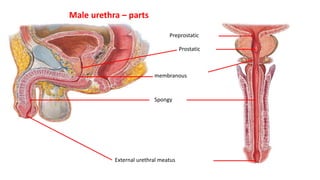
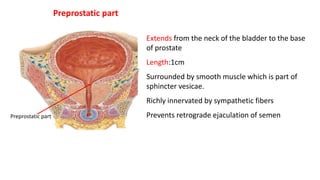
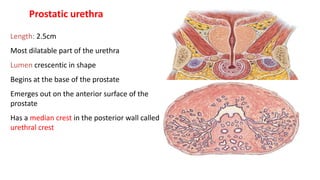
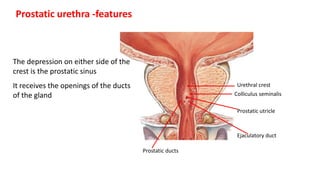
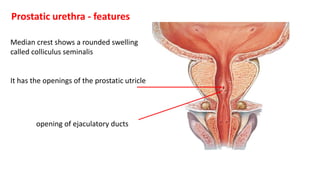
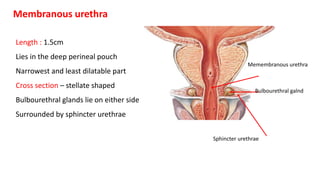
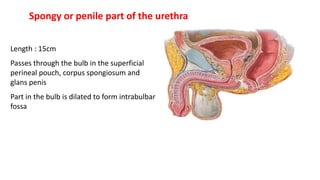
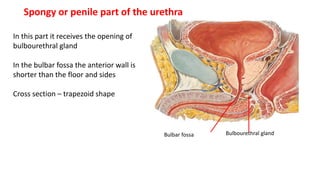
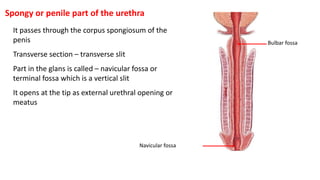
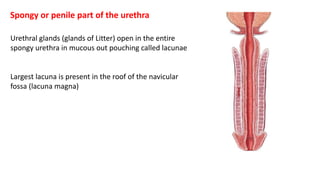
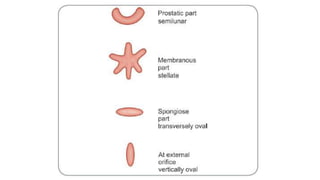
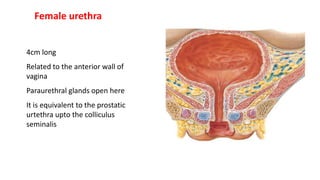
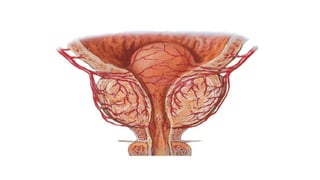
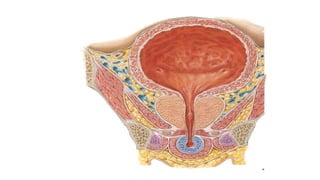
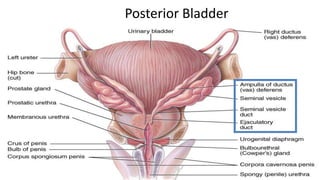
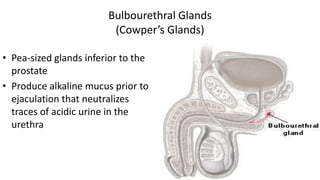
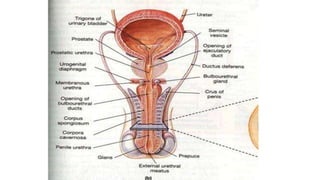
The document provides a comprehensive overview of the prostate gland, detailing its anatomy, relations, lobes, blood supply, development, and associated pathologies, such as benign hypertrophy and prostate cancer. It also covers the anatomical features of the male and female urethra, including the bulbourethral glands, and their roles in the reproductive system. The information emphasizes the importance of prostate health and potential symptoms of prostate conditions.