The document discusses the key aspects of general anesthesia, including:
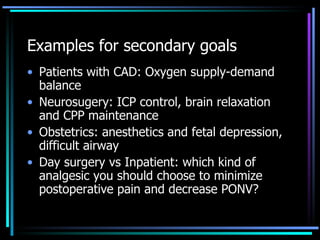
1) An overview of general anesthesia, its goals of safety, amnesia, hypnosis, and analgesia.
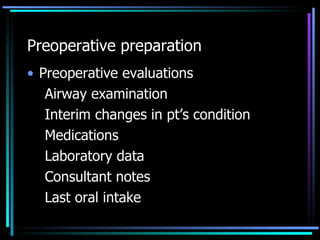
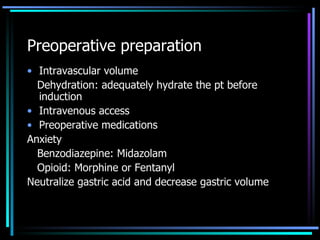
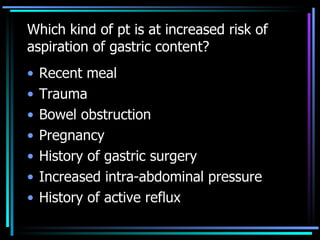
2) Preoperative preparation such as evaluations, medications, and ensuring adequate hydration and intravenous access.
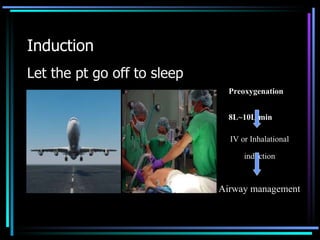
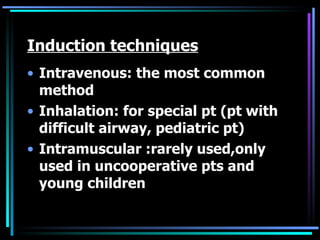
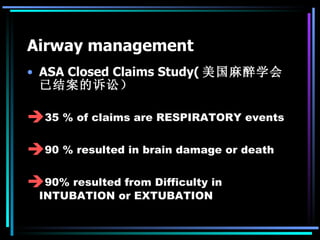
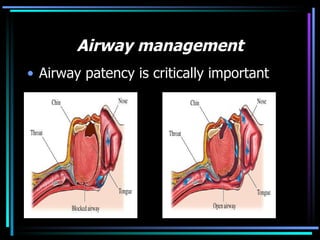
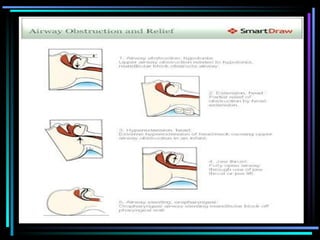
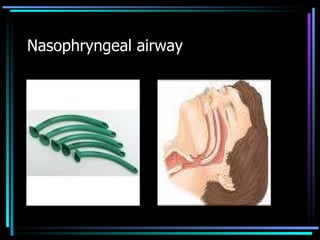
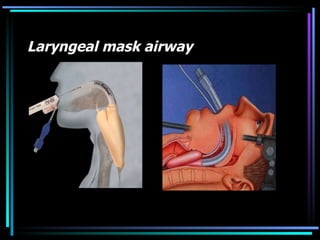
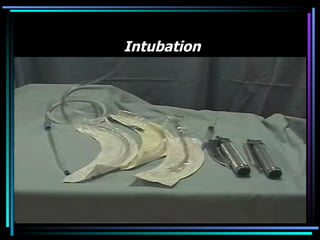
3) Induction of anesthesia through preoxygenation, intravenous or inhalational methods, and airway management including intubation.
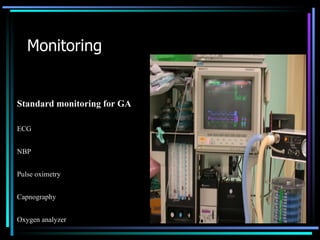
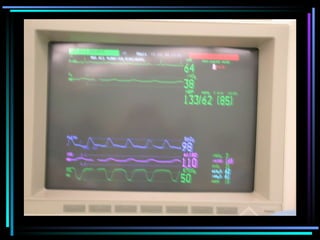
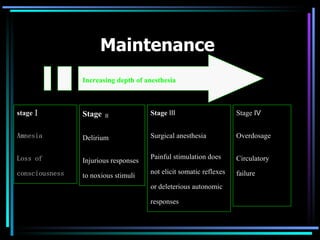
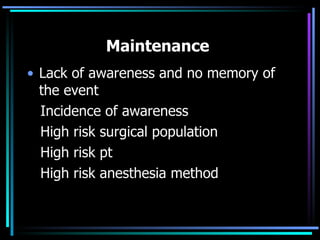
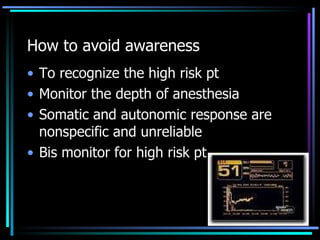
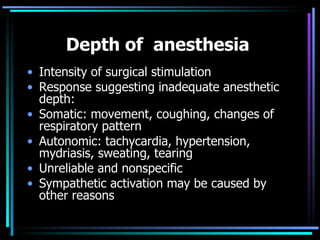
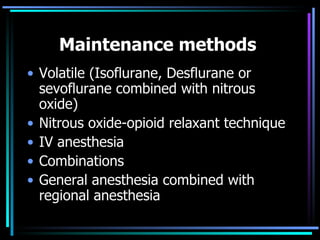
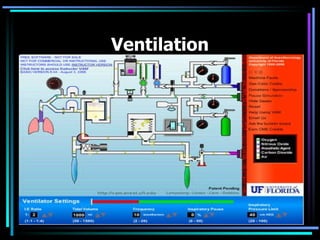
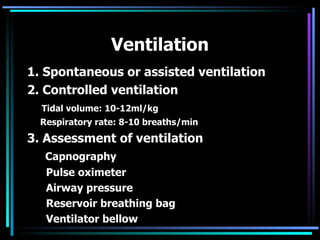
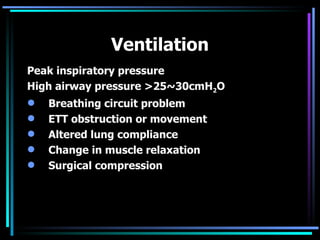
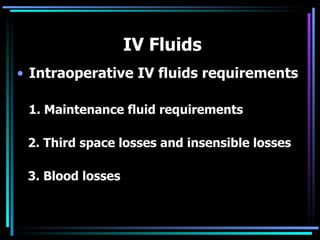
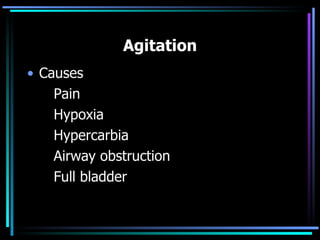
4) Maintenance of anesthesia by maintaining homeostasis, monitoring depth to prevent awareness, and using various anesthetic methods and ventilation techniques.
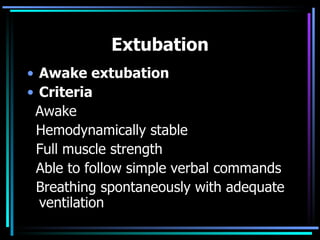
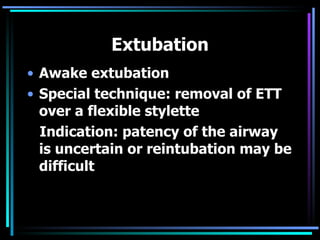
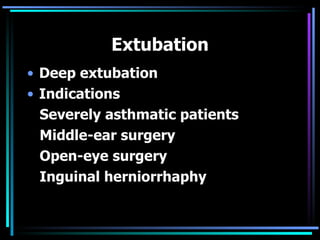
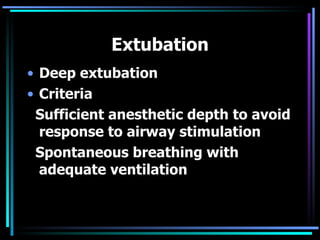
5) Emergence from anesthesia and considerations for extubation such as ensuring the patient is awake, responsive, and has adequate pain