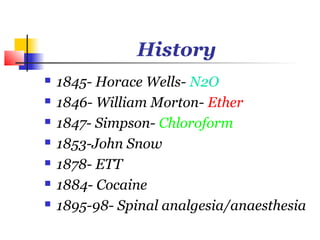
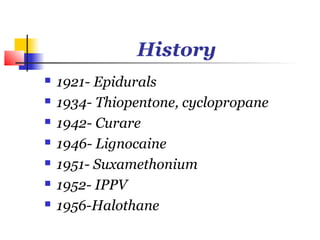
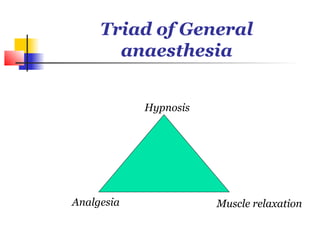
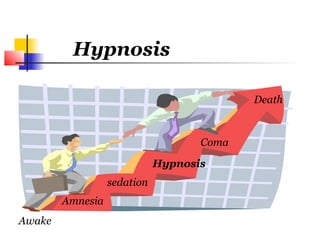
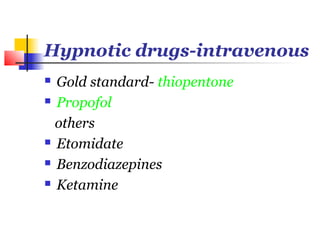
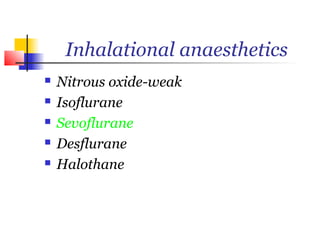
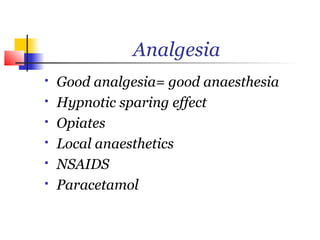
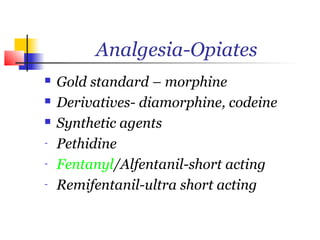
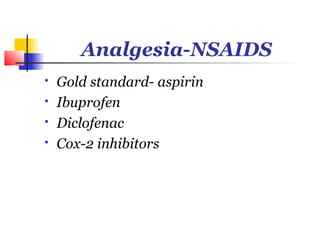
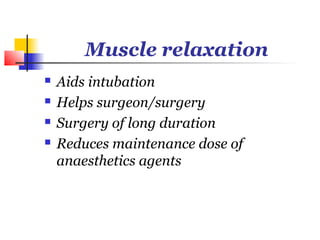
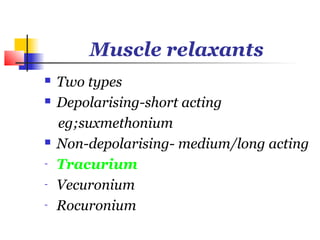
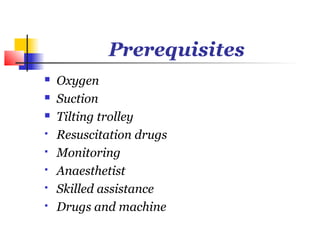
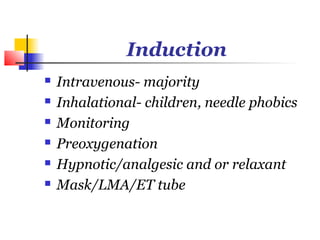
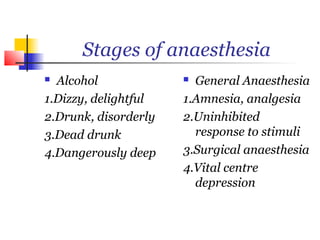
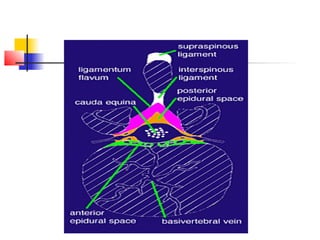
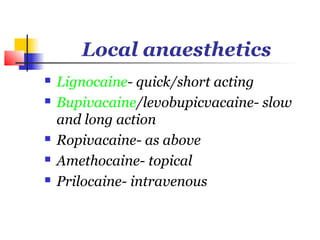
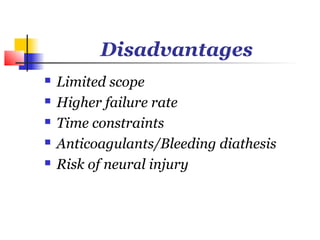
The document provides a comprehensive overview of the types and history of anaesthesia, including significant historical milestones and the development of various anaesthetic agents. It outlines the definitions and classifications of general, regional, and local anaesthesia while discussing the phases and procedures involved in general anaesthesia. Additionally, the document highlights the advantages and disadvantages of each anaesthesia type, mentioning key drug classes and their applications.