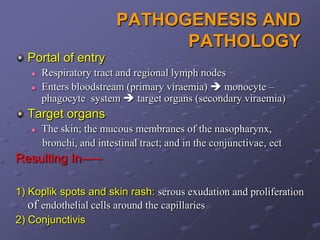
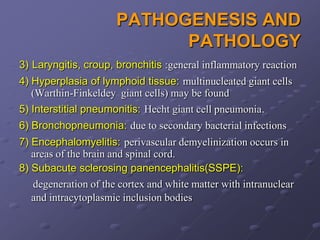
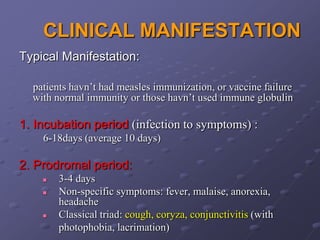
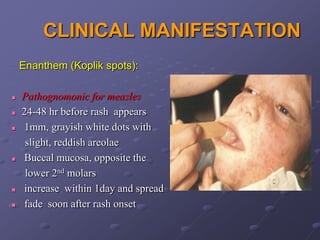
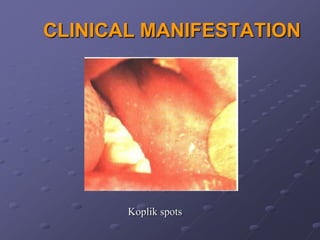
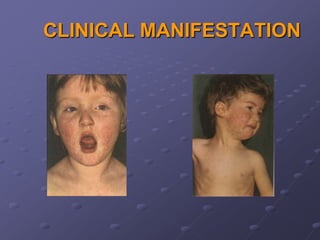
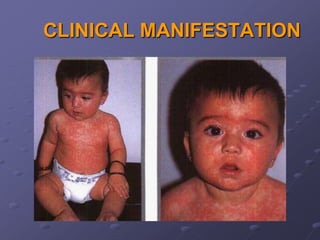
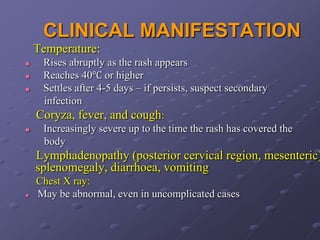
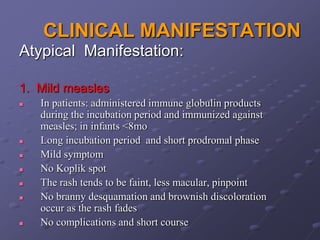
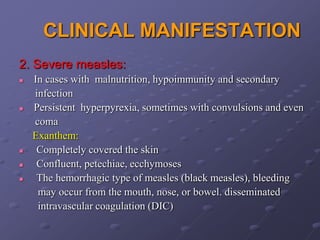
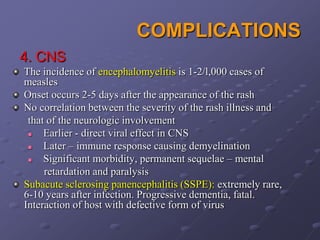
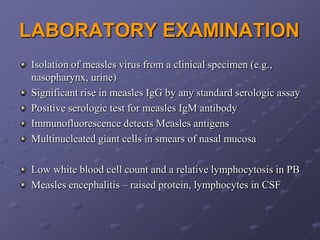
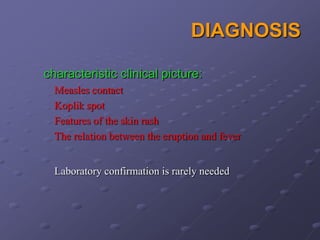
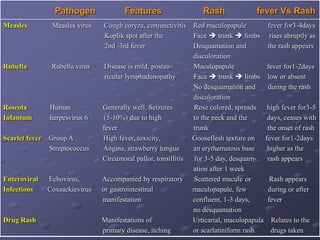
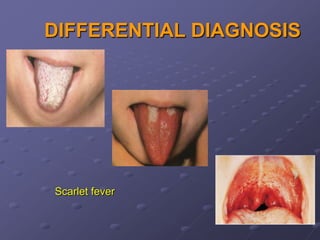
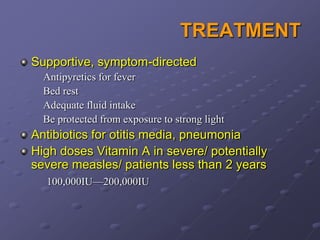
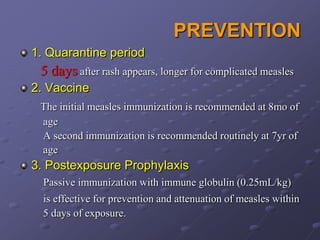
Measles is a highly contagious viral infection characterized by a maculopapular rash. It is caused by measles virus and spreads through respiratory droplets. Common symptoms include fever, cough, coryza, and conjunctivitis. Koplik spots may appear in the mouth before the rash. Complications can include pneumonia, encephalitis, and subacute sclerosing panencephalitis. Diagnosis is usually based on clinical presentation. Treatment focuses on relieving symptoms, with supportive care and antibiotics for secondary infections. Prevention involves vaccination and quarantine after exposure.