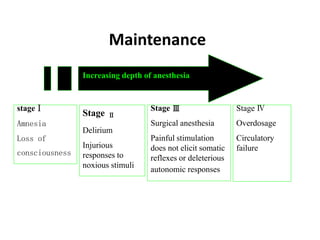
This document provides an overview of general anesthesia. It defines general anesthesia as a reversible state of unconsciousness with inability to respond to pain. It then briefly discusses the history of general anesthesia and compares it to local anesthesia and conscious sedation. The rest of the document details various aspects of general anesthesia including pre-anesthetic checkups, airway assessments, induction, maintenance, emergence, postoperative care, complications and their management, as well as advantages, disadvantages, contraindications and indications for general anesthesia.