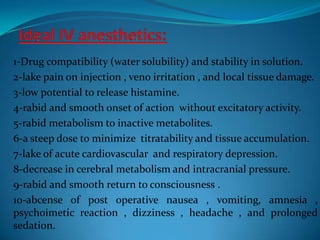
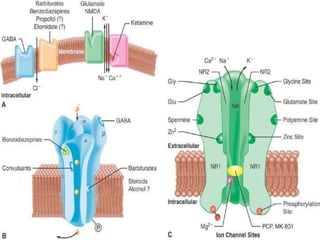
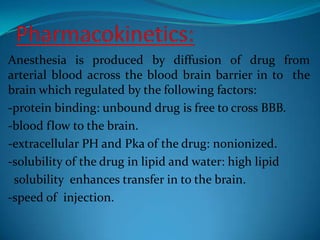
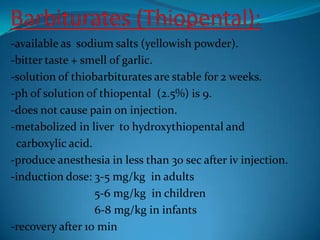
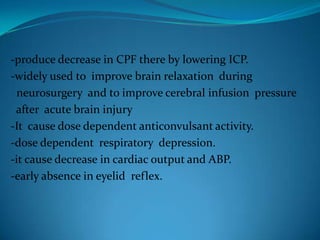
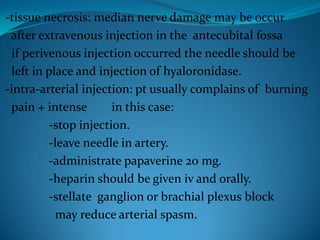
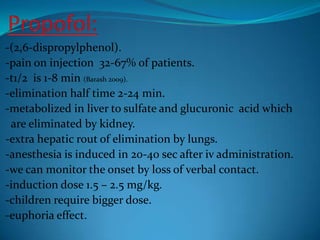
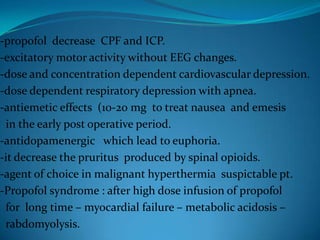
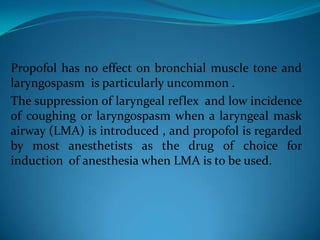
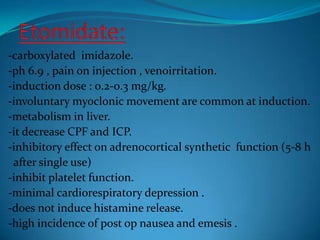
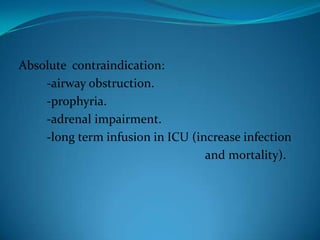
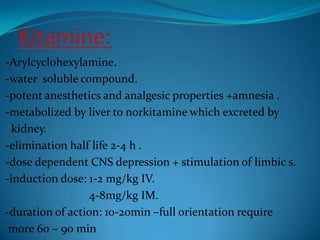
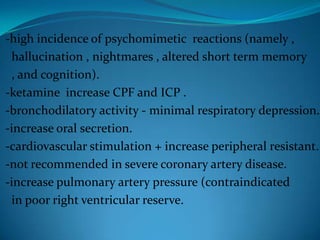
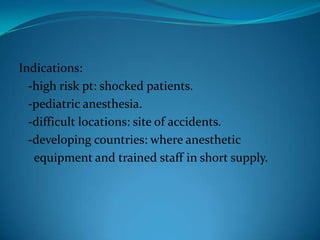
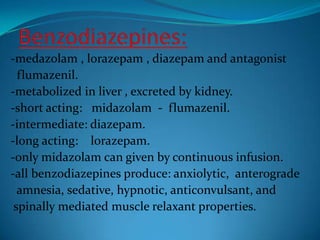
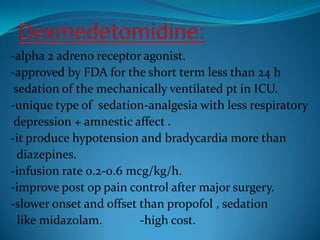
The document discusses ideal properties of intravenous anesthetics and summarizes the pharmacokinetics and pharmacodynamics of several commonly used IV anesthetics including barbiturates, propofol, etomidate, ketamine, benzodiazepines, and dexmedetomidine. It outlines desirable traits such as rapid onset and offset of action, minimal cardiovascular and respiratory depression, and lack of adverse effects. Each drug's mechanism of action, dosing, metabolism, indications, contraindications, and side effects are briefly described.