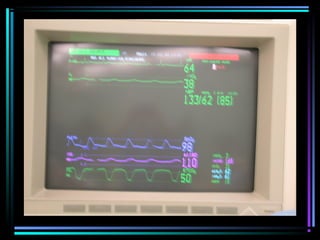
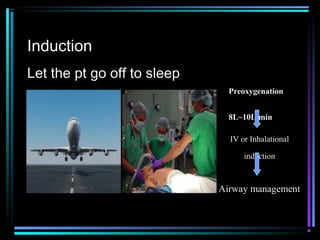
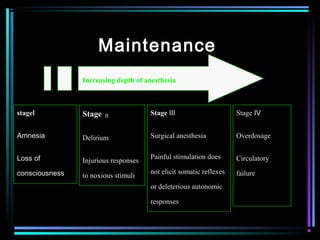
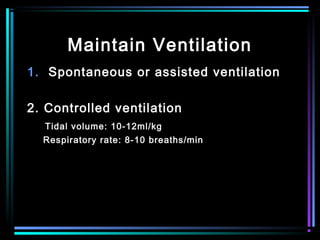
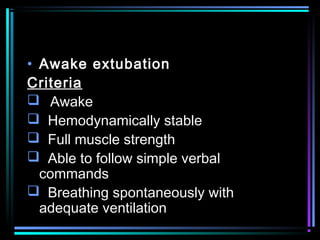
General anesthesia involves inducing a state of unconsciousness during surgery through the use of drugs. The goals are amnesia, hypnosis, analgesia, and immobility. Preparation includes evaluations of the patient's airway, medical conditions, medications, and labs. Monitoring is established and intravenous access and fluids are given. Induction involves preoxygenation before administering intravenous or inhalational drugs to induce unconsciousness and allow intubation. Maintenance of anesthesia involves increasing the depth of unconsciousness through volatile gases, IV drugs, or combinations while monitoring vital signs and homeostasis. Emergence and extubation involve ensuring the patient meets criteria like being awake, responsive, with full strength before discharge from recovery. Transport is the