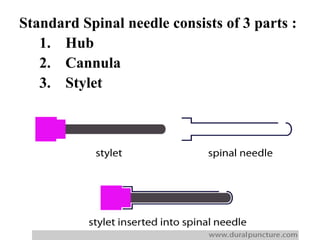
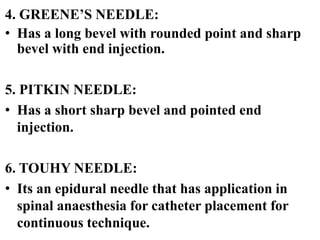
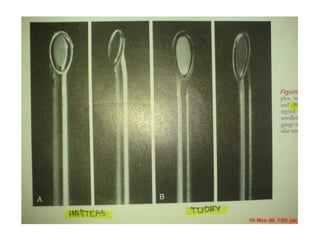
This document discusses the history and types of spinal and epidural needles. It begins by introducing regional anesthesia and the importance of needles. It then describes the development of spinal needles over time from Quincke's original design to modern pencil-point needles. Key spinal needle types including Quincke, Whitacre, and Sprotte are outlined. Epidural needles including Touhy and Crawford designs are also summarized. Complications related to needle placement are briefly mentioned. The document emphasizes that needle design modifications have improved techniques like spinal and epidural anesthesia.