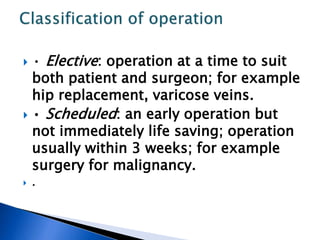
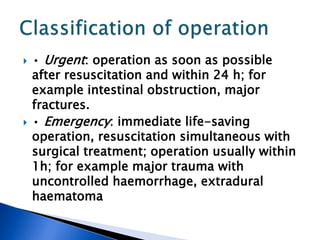
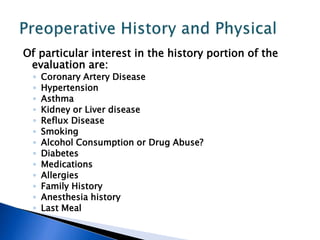
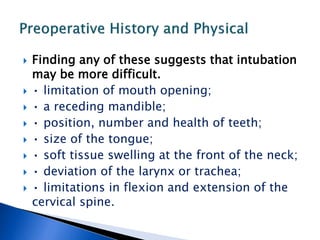
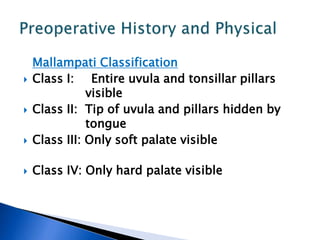
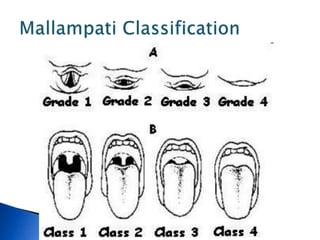
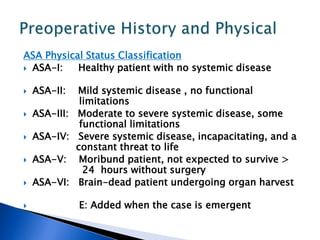
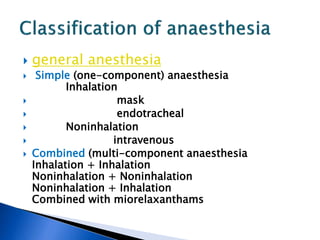
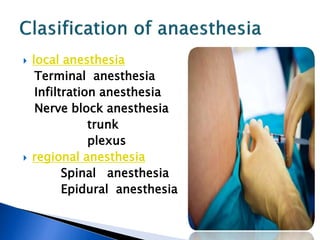
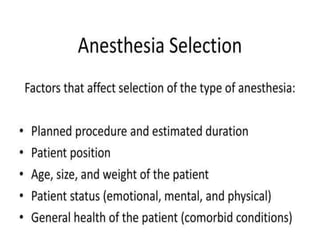
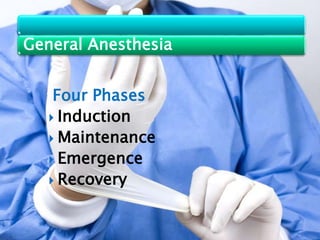
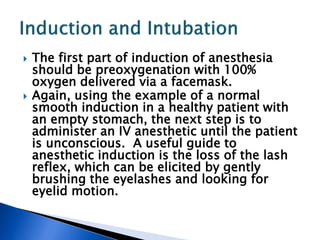
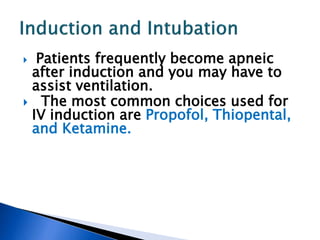
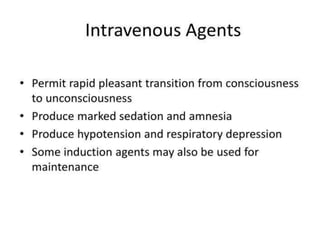
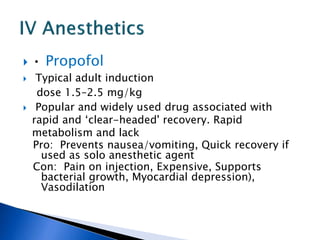
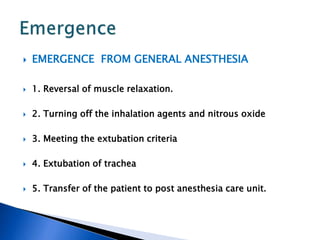
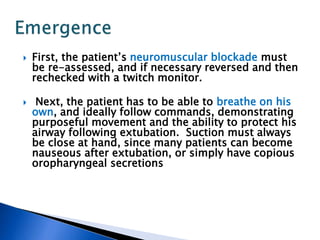
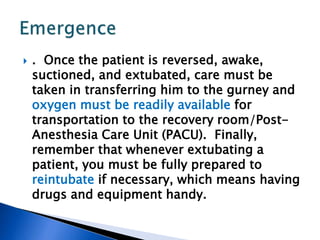
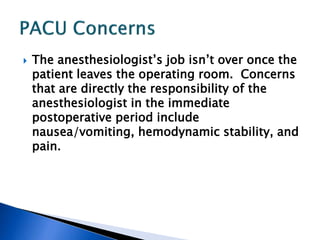
This document provides an overview of general principles of anesthesiology for 5-year medical students. It discusses topics like preoperative history and physical exams, IV access and premedication, room setup and monitors, induction and intubation, and postoperative care. The preoperative evaluation focuses on assessing risk factors and the airway. Proper equipment and monitor setup is emphasized prior to patient arrival. Common induction agents and intubation techniques are also reviewed.