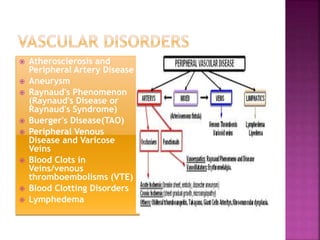
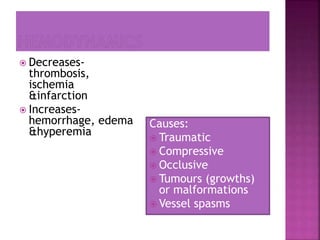
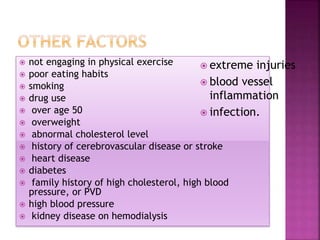
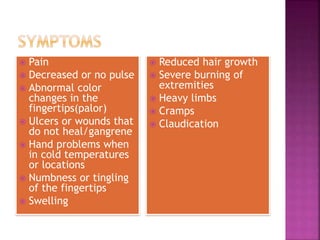
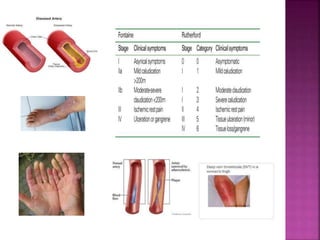
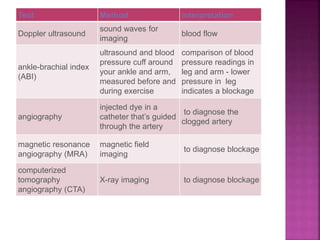
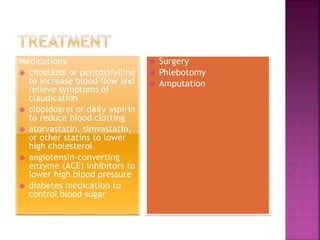
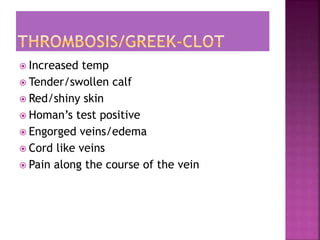
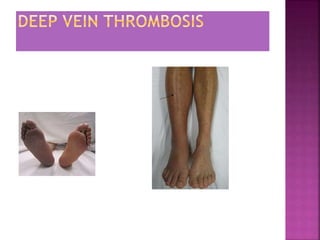
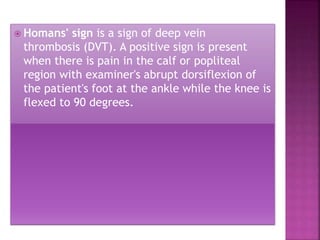
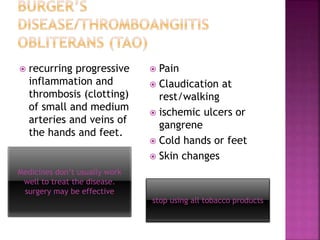
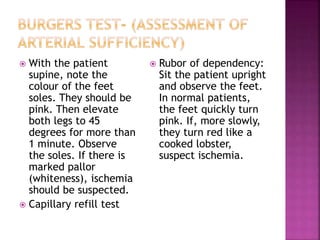
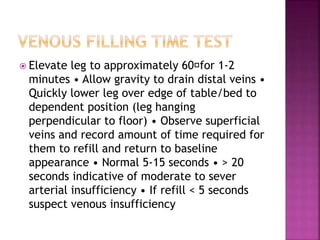
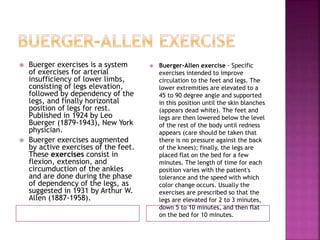
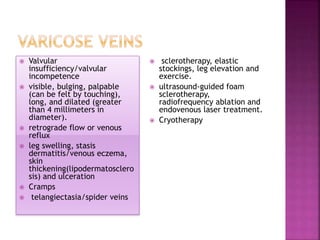
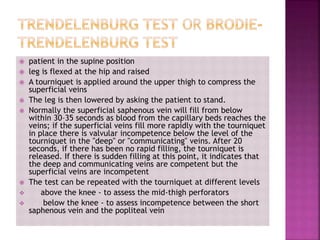
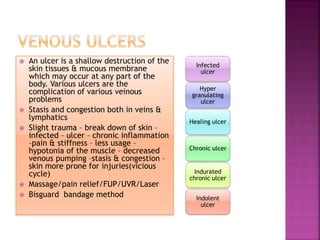
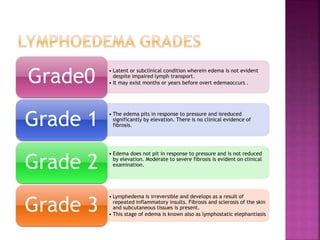
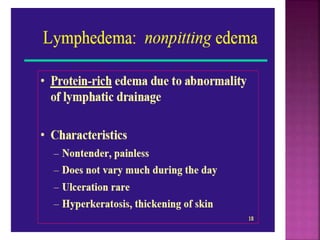
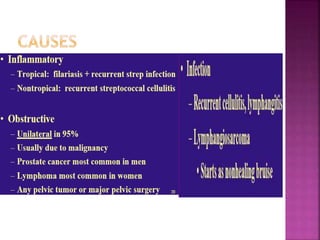
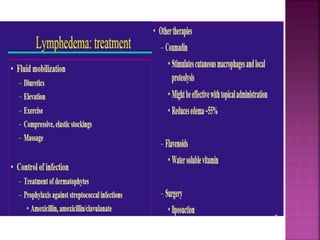
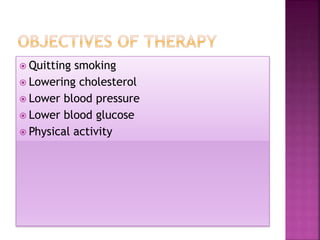
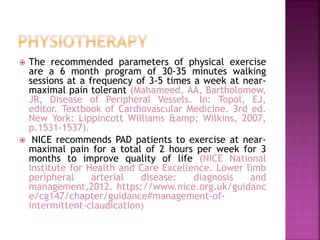
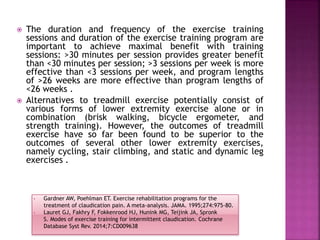
This document discusses peripheral vascular disease and its management. It covers topics such as thrombosis, varicose veins, deep vein thrombosis, peripheral artery disease, aneurysms, Raynaud's phenomenon, Buerger's disease, venous disease, blood clots, lymphedema, risk factors, symptoms, diagnostic tests including Doppler ultrasound, ankle-brachial index, angiography and treatments including medications, surgery, and lifestyle changes like exercise and smoking cessation.
![ Management of vascular disease[8 Hours]:
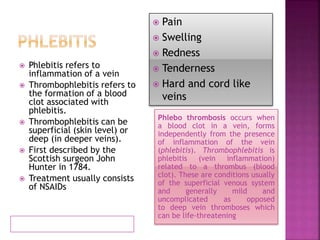
thrombosis, phlebitis and phlebothrombosis,
burger’s disease, varicose veins, DVT, venous
ulcers, lymphoedema & its PT management](https://image.slidesharecdn.com/vasculardisorders-160920130338/85/Vascular-disorders-2-320.jpg)