1) Pyogenic meningitis is an inflammation of the membranes surrounding the brain and spinal cord caused most commonly by bacterial infection in infants and young children.
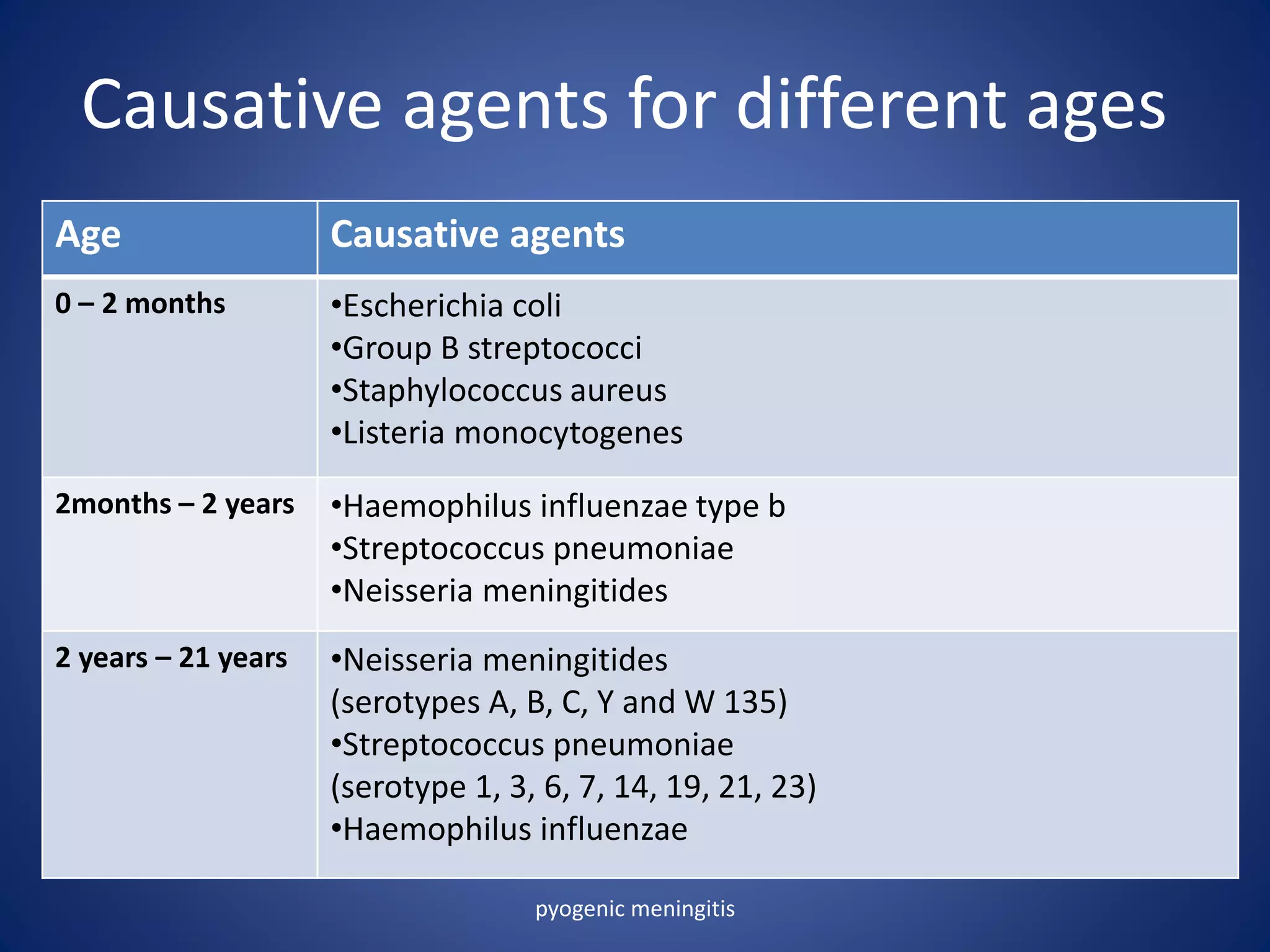
2) The causative agents vary by age but include Escherichia coli, Group B Streptococci, Staphylococcus aureus, and Listeria monocytogenes in infants under 2 months. Haemophilus influenzae type b and Streptococcus pneumoniae are common causes in children from 2 months to 2 years.
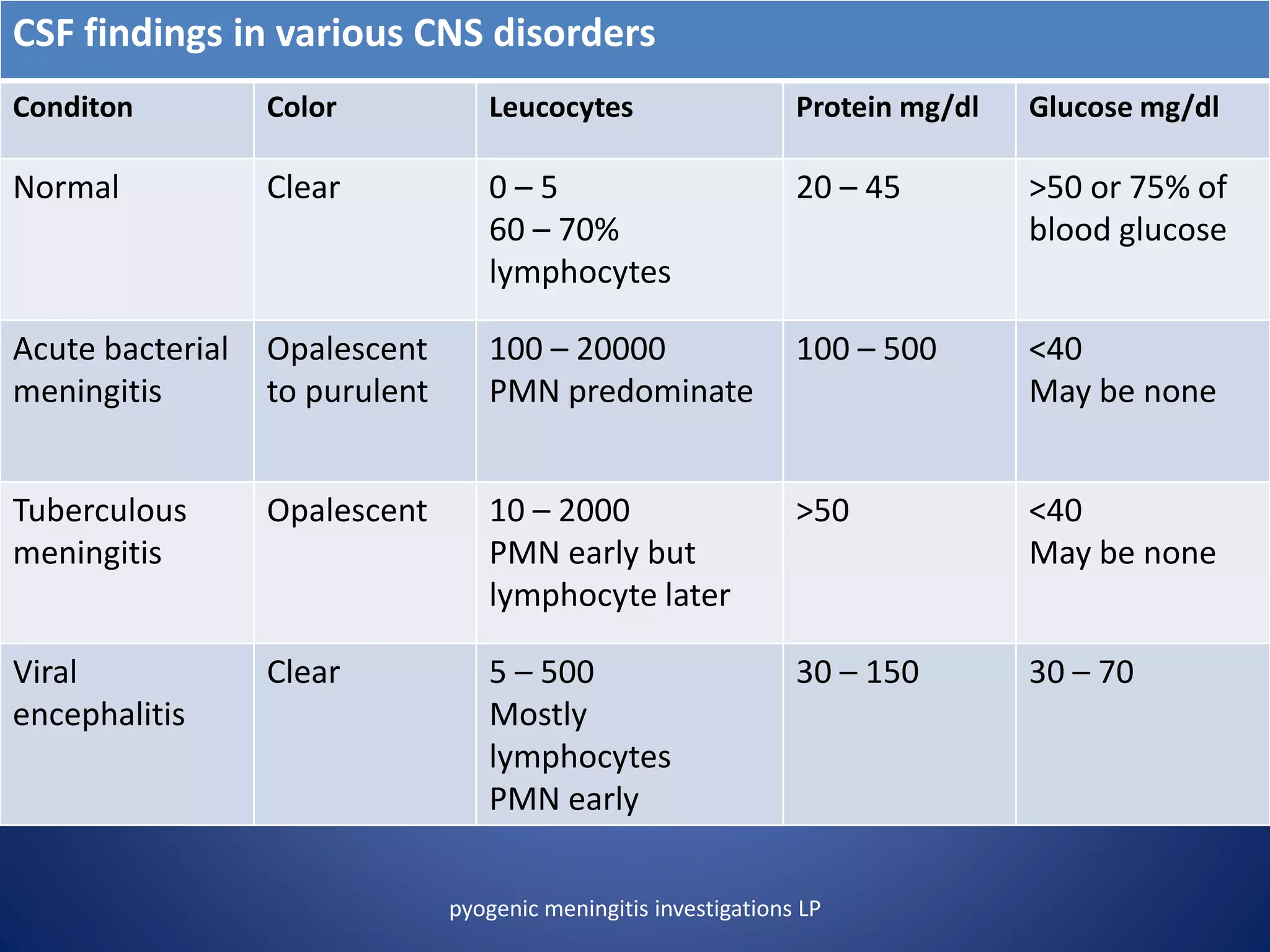
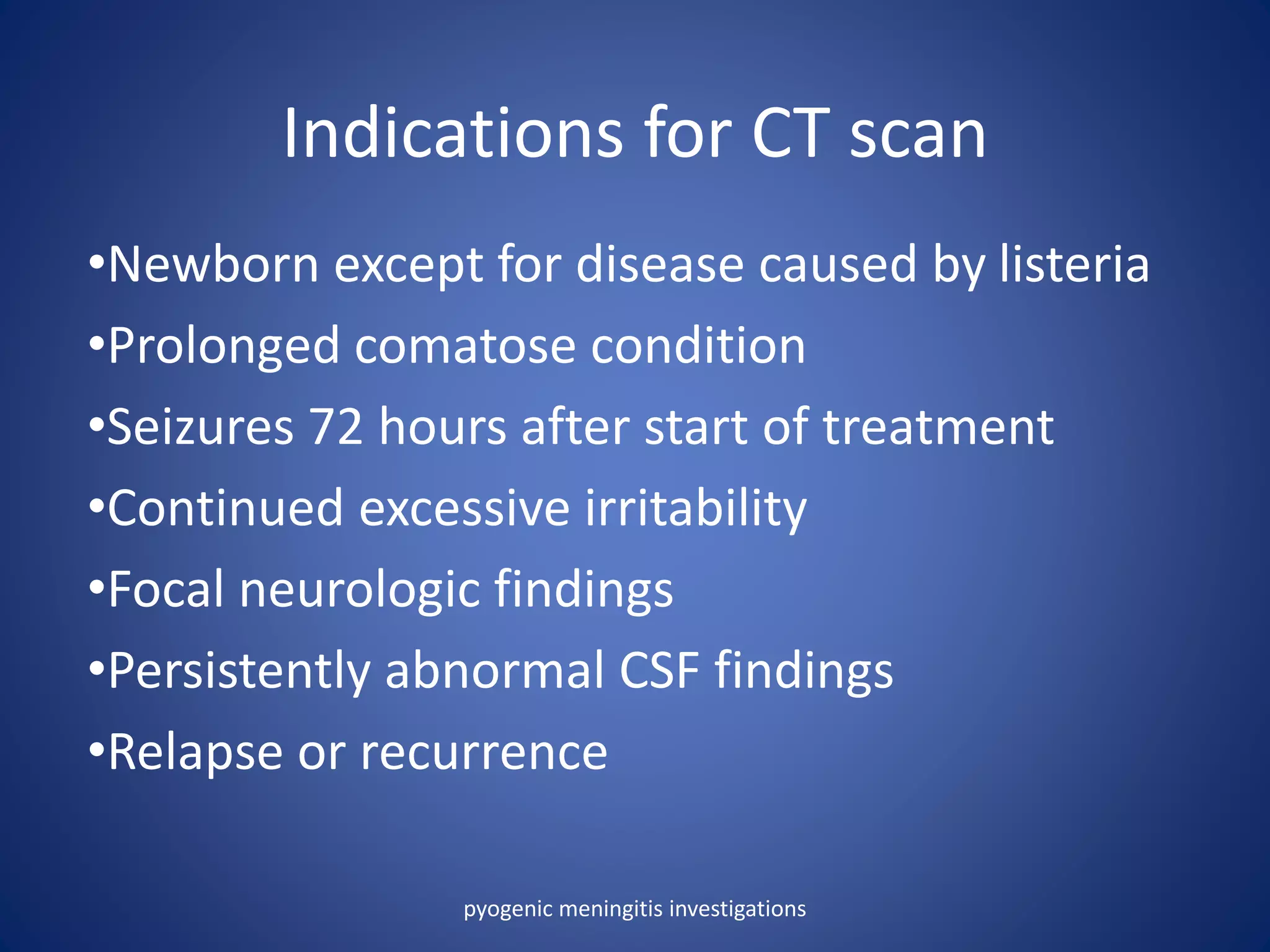
3) Clinical features include fever, irritability, vomiting, seizures, and bulging fontanelle. Diagnosis involves lumbar puncture to examine cerebrospinal fluid for presence of bacteria, white blood cells and