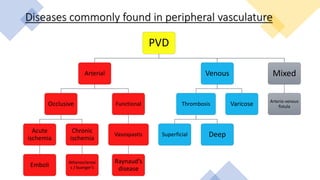
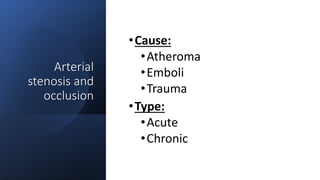
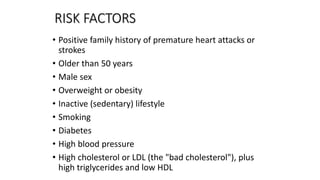
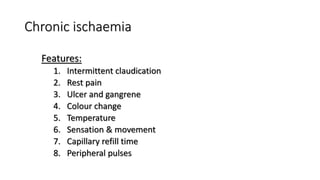
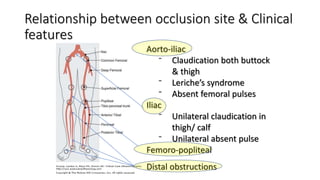
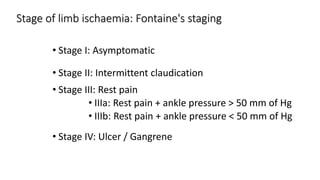
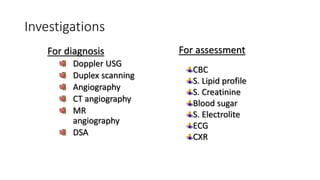
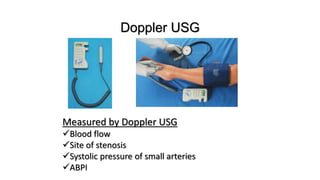
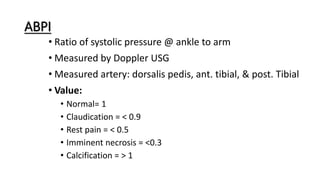
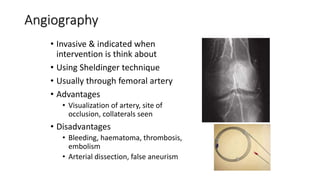
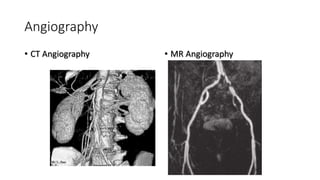
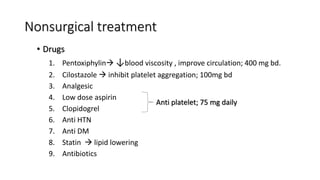
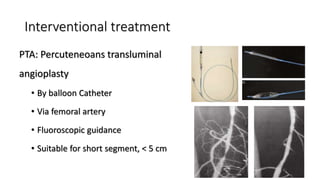
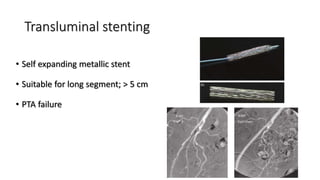
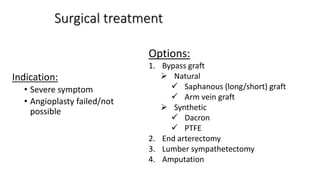
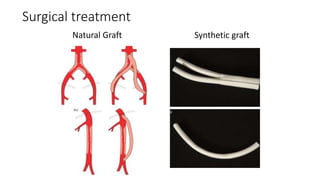
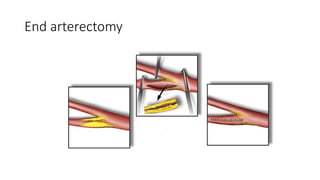
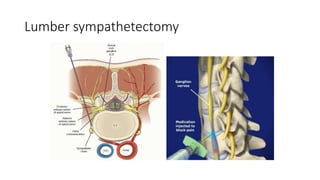
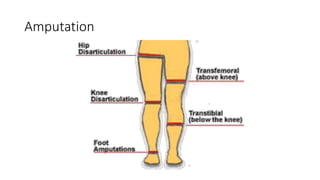
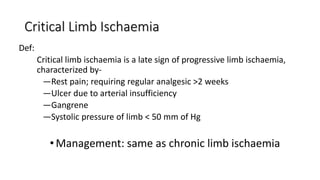
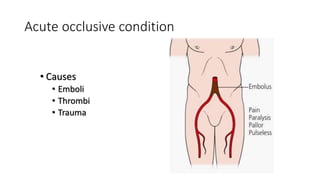
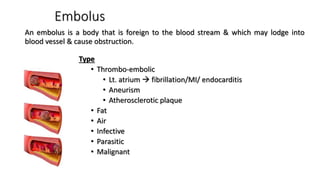
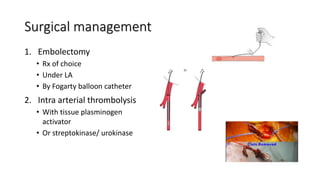
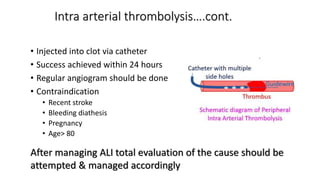
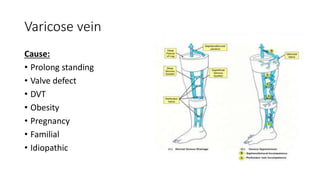
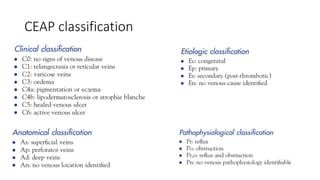
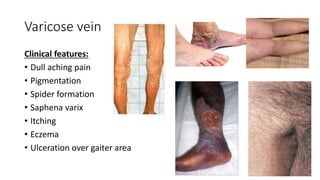
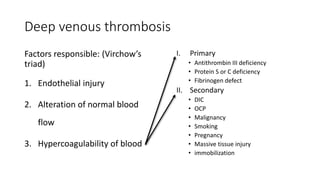
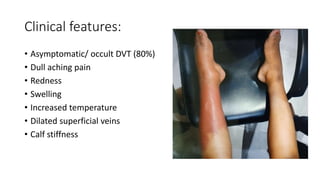
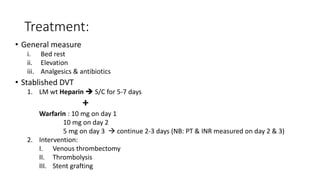
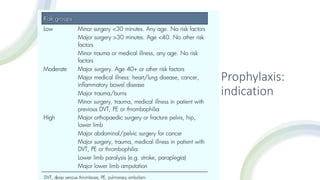
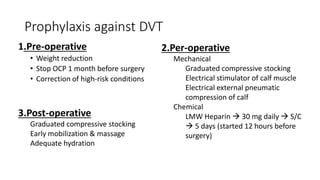
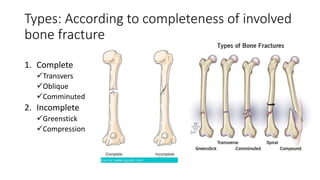
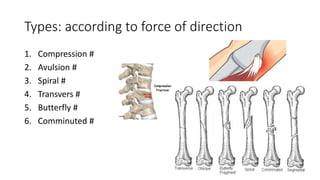
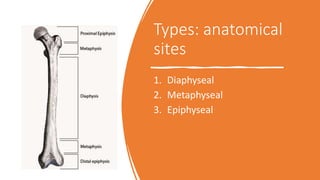
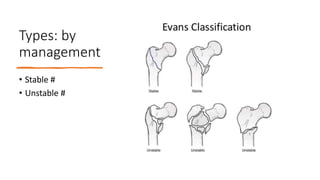
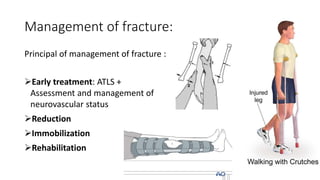
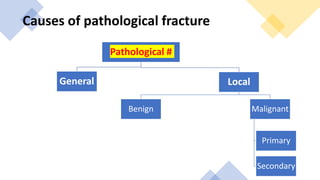
The document provides an outline for a class on final proficiency examinations covering vascular disease and orthopedics. The vascular disease section includes topics like peripheral vascular disease, arterial diseases like acute and chronic limb ischemia, venous diseases like varicose veins and deep vein thrombosis. The orthopedics section covers fractures, their classification, diagnosis and management. Key investigations discussed are Doppler ultrasound, angiography and management includes nonsurgical options like medications and interventional procedures like angioplasty as well as surgical treatments.