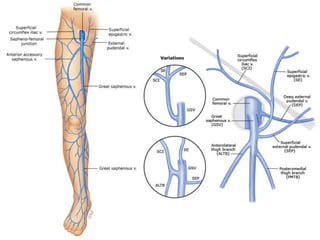
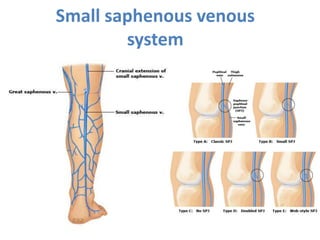
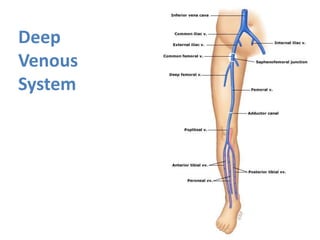
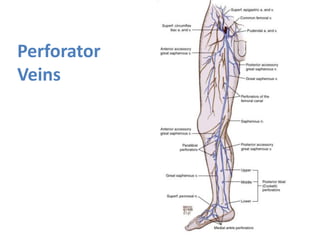
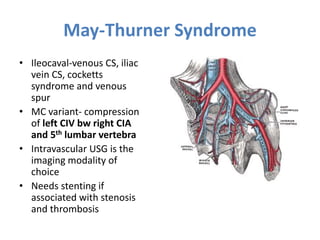
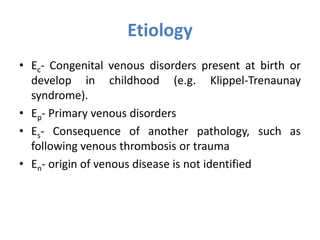
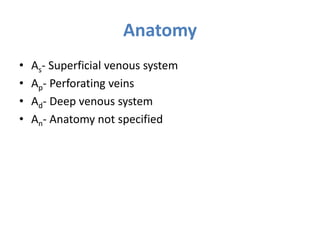
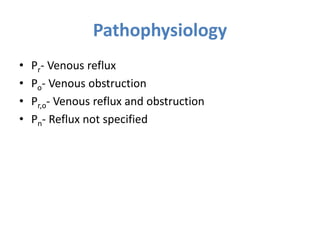
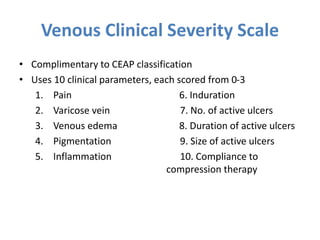
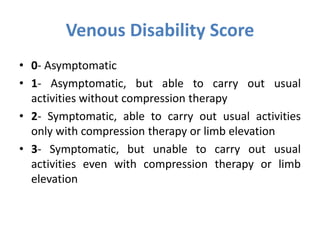
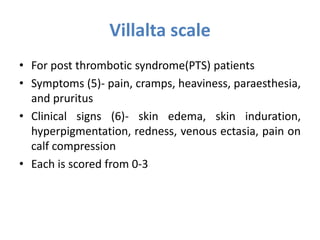
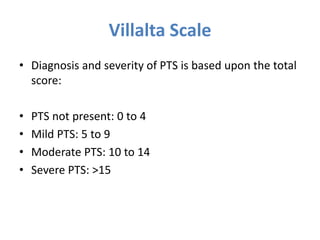
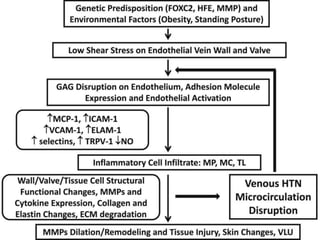
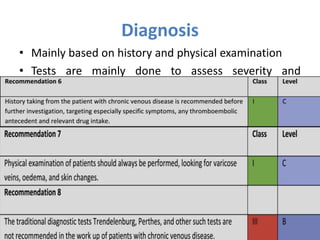
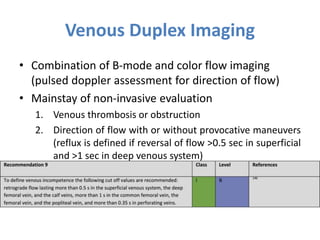
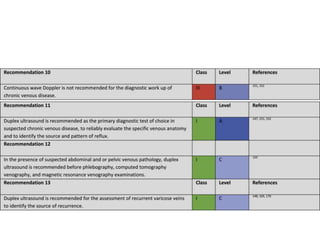
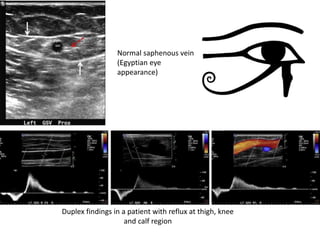
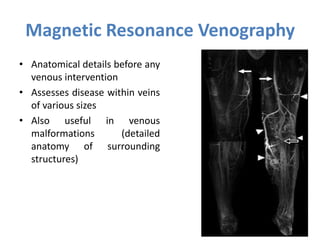
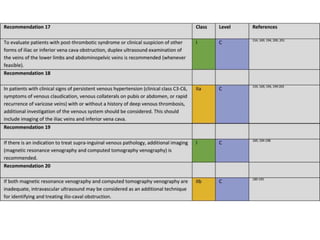
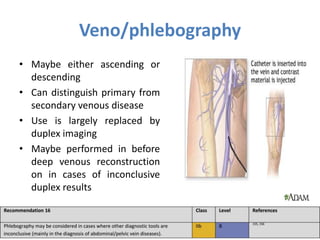
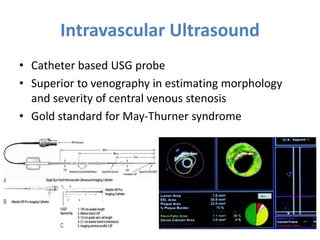
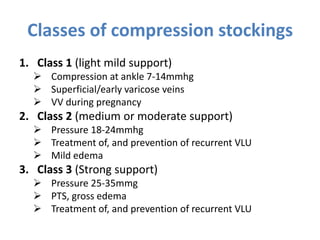
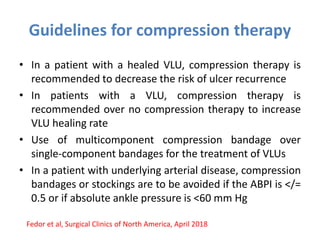
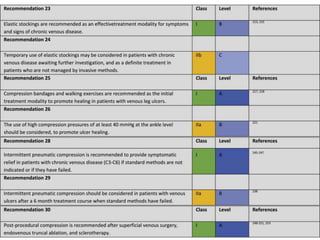
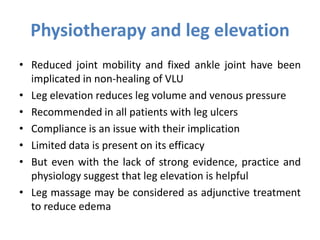
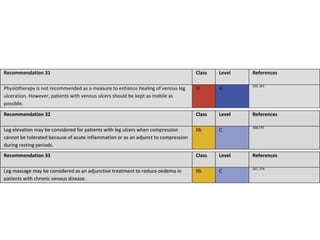
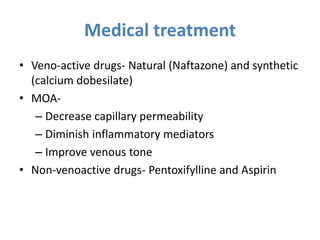
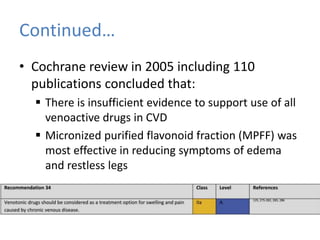
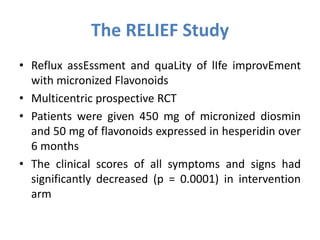
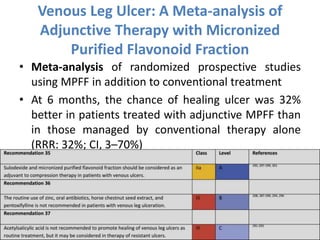
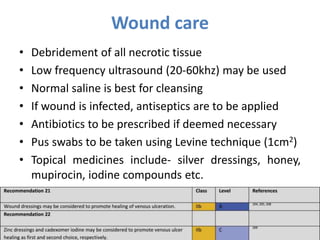
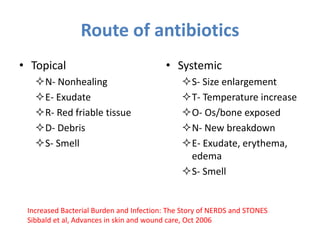
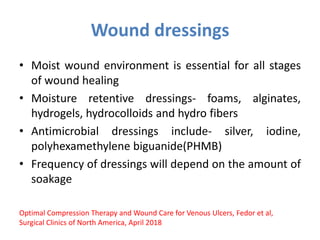
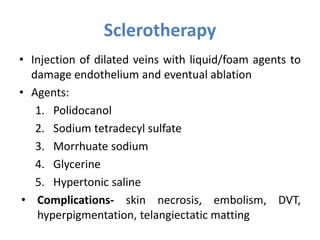
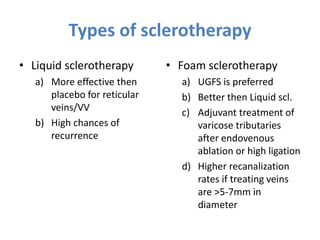
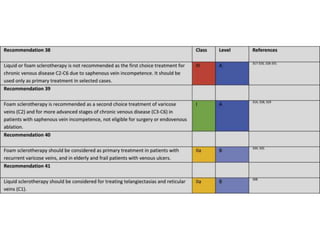
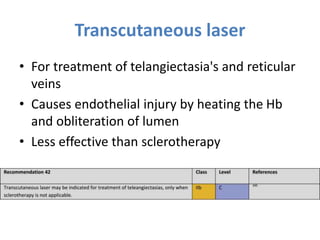
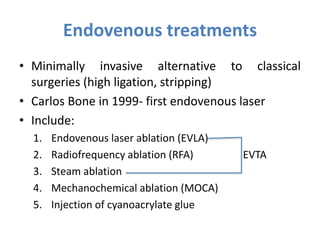
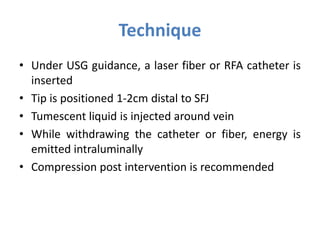
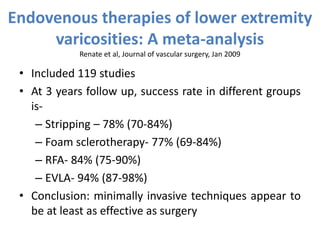
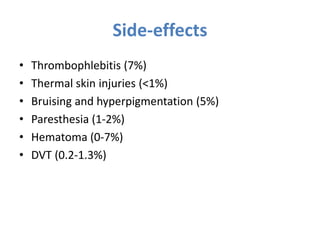
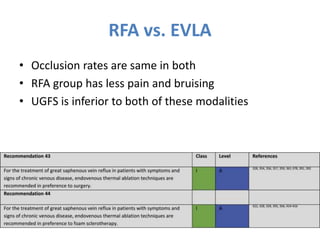
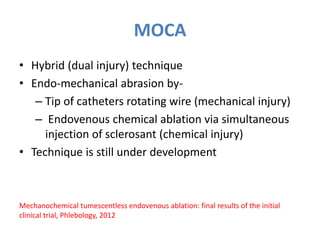
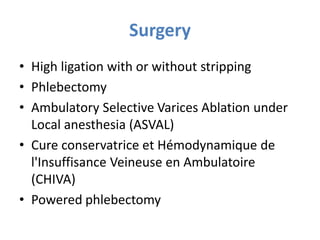
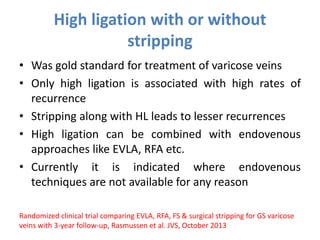
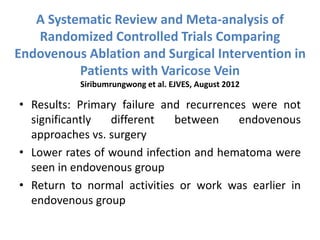
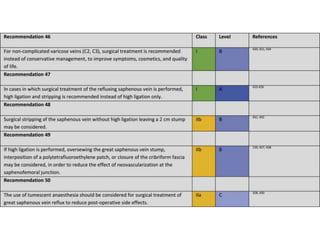
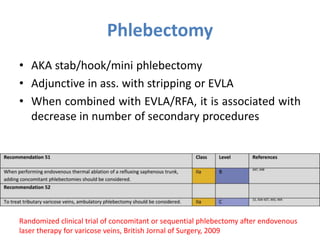
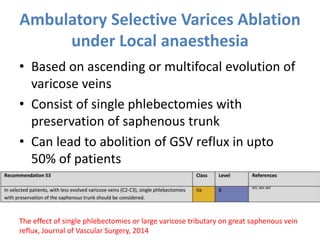
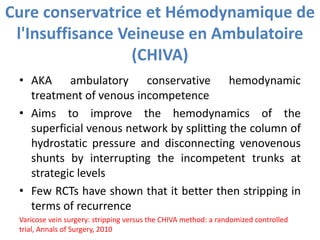
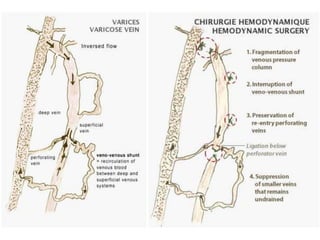
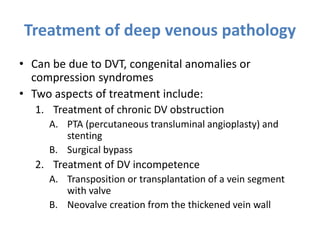
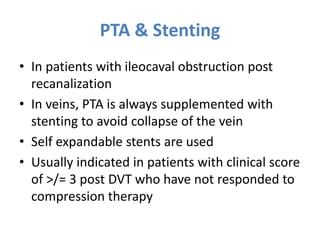
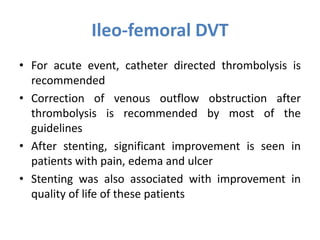
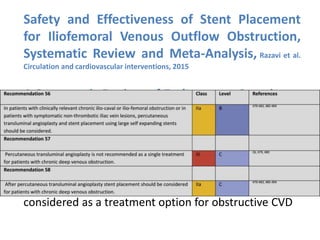
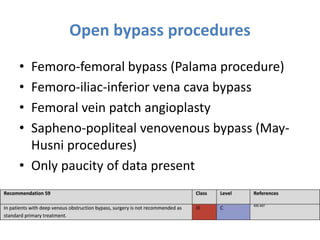
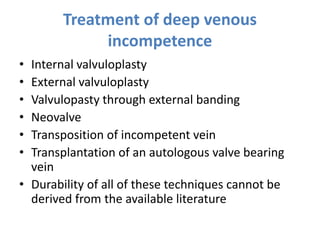
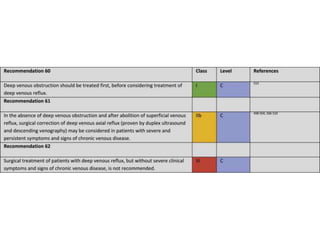
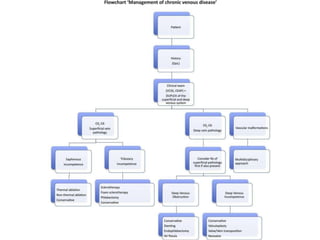
This document discusses the management of chronic venous insufficiency. It begins by defining key terms like chronic venous disorder, chronic venous disease, and chronic venous insufficiency. It then covers the history, anatomy, pathophysiology, classification systems, clinical manifestations, diagnosis, and treatment of chronic venous insufficiency. For diagnosis, it discusses tests like duplex ultrasound, CT, MRI, and angiography. For treatment, it covers conservative options like compression therapy, medications, wound care and dressings. It also discusses interventional options like sclerotherapy, laser ablation, radiofrequency ablation, foam sclerotherapy, and surgery.