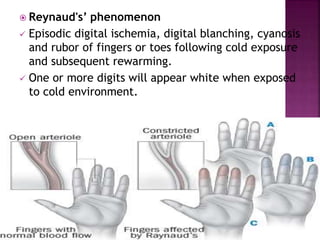
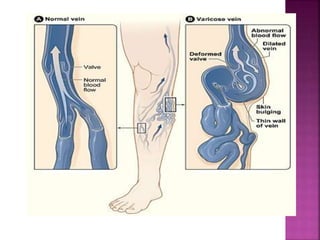
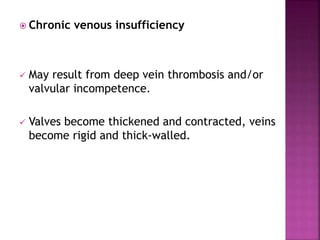
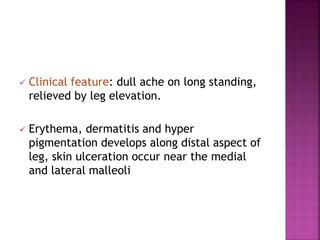
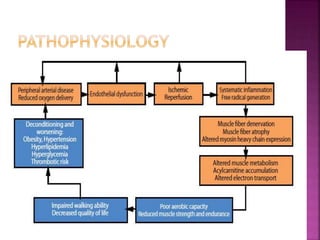
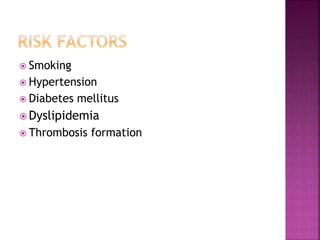
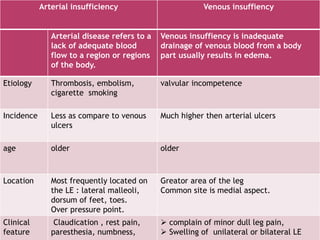
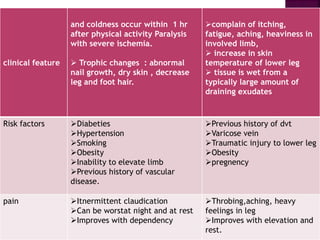
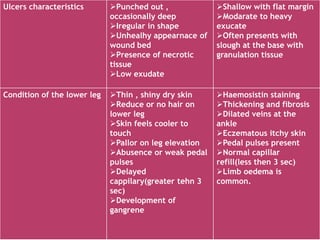
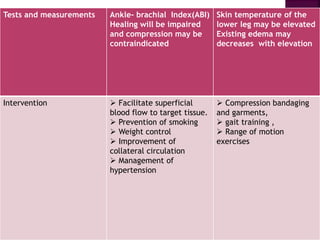
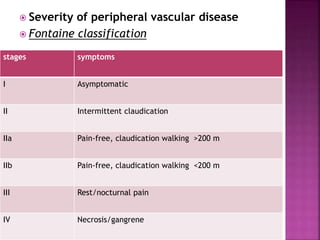
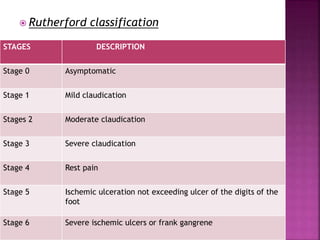
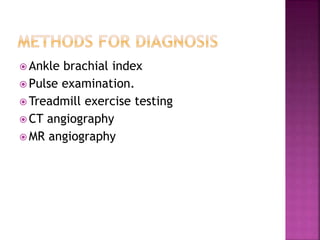
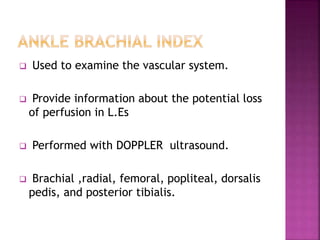
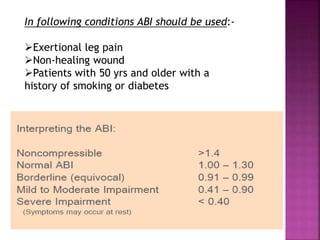
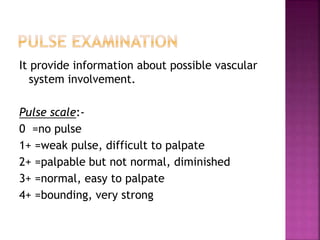
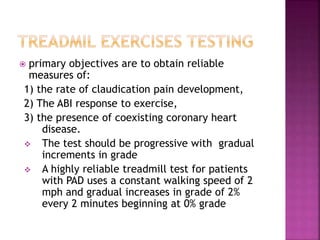
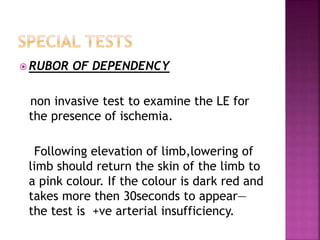
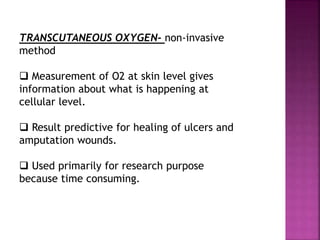
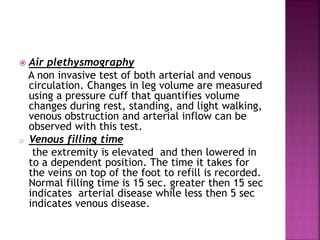
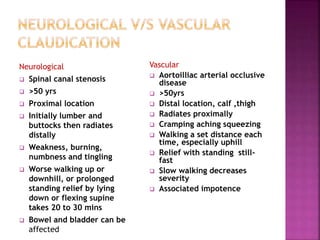
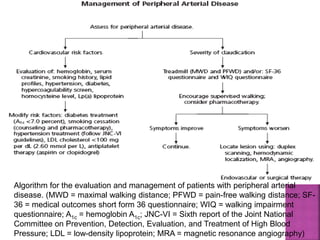
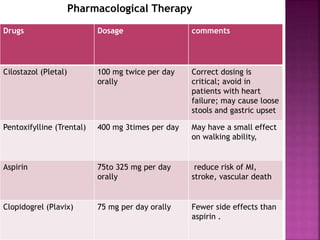
This document summarizes peripheral vascular diseases that affect arterial and venous blood flow in the extremities. It discusses various arterial disorders like fibro muscular dysplasia, thromboanginitis obliterans, acute arterial occlusion, atheroembolism, and Reynaud's phenomenon. It also covers various venous disorders including deep vein thrombosis, superficial vein thrombosis, varicose veins, and chronic venous insufficiency. Risk factors, clinical features, diagnostic tests, and management approaches are described for different peripheral vascular conditions.