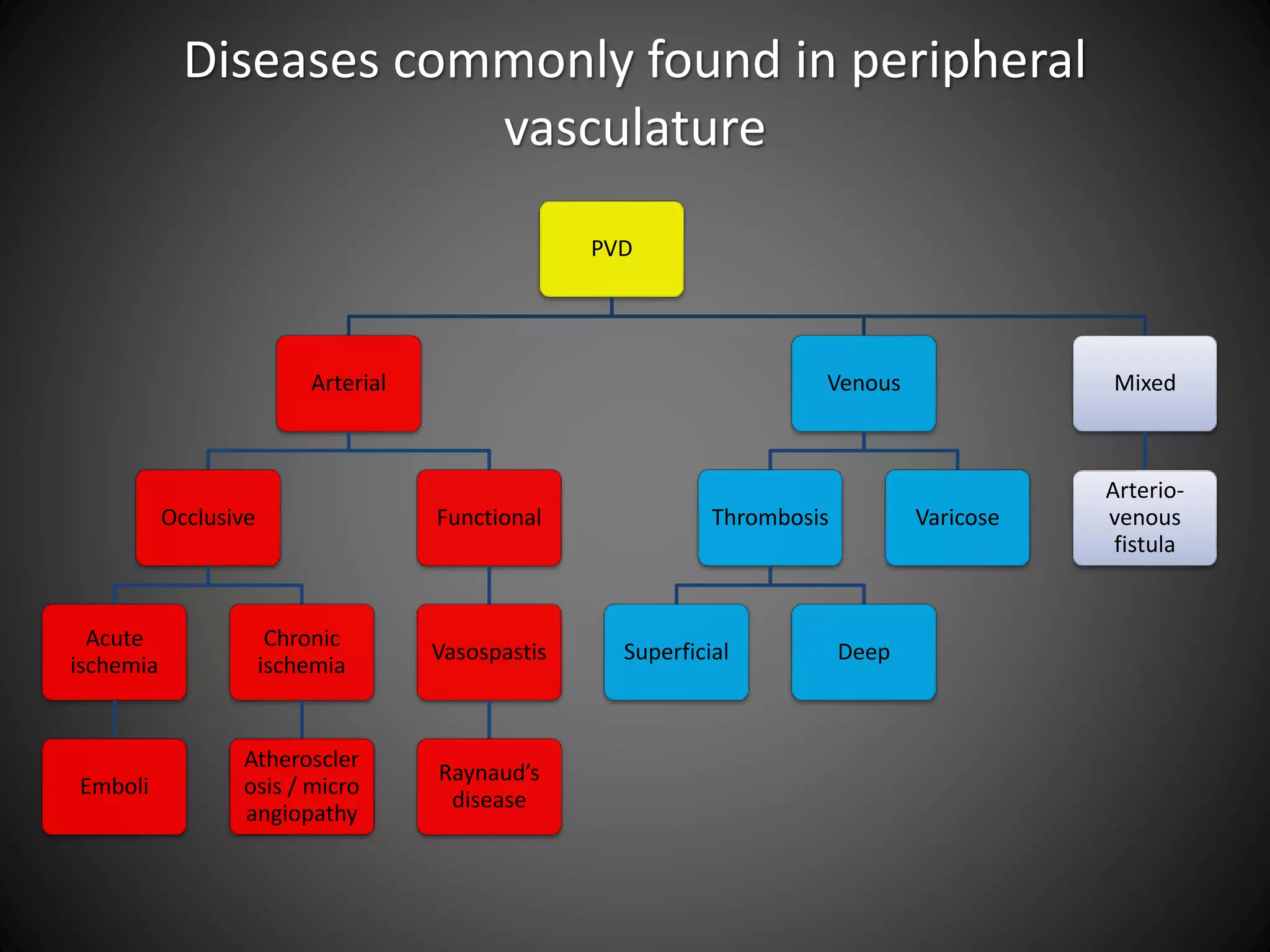
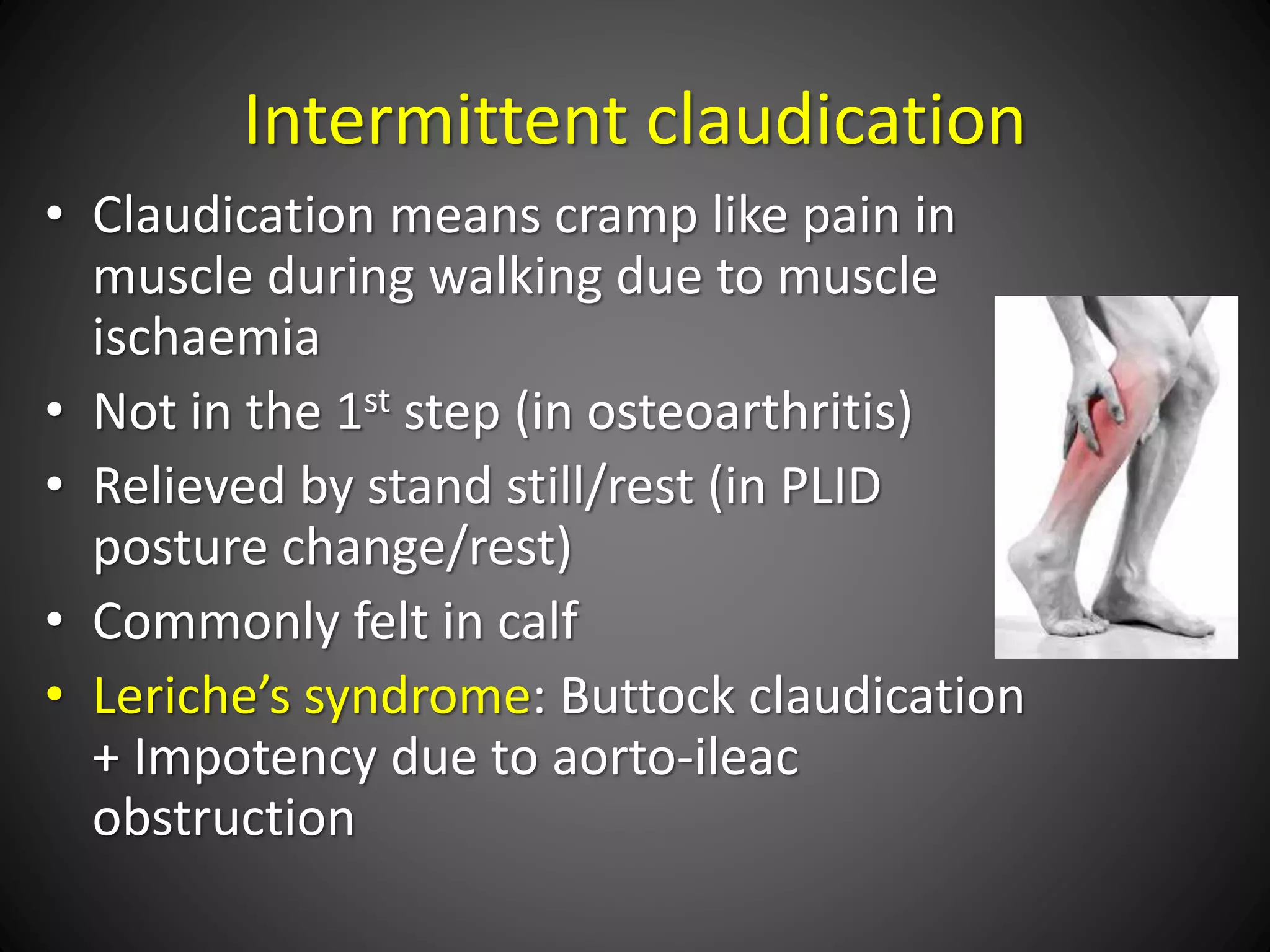
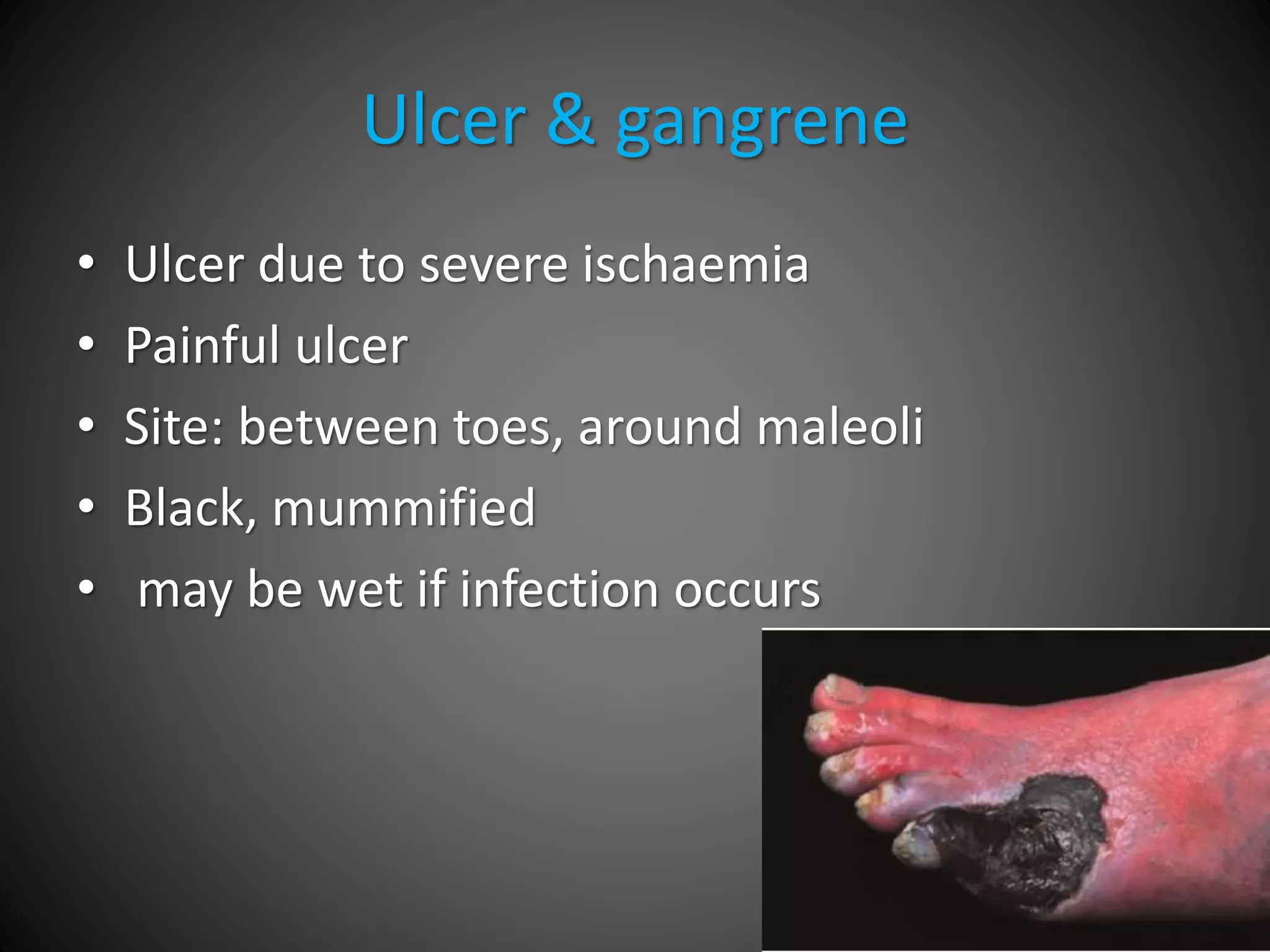
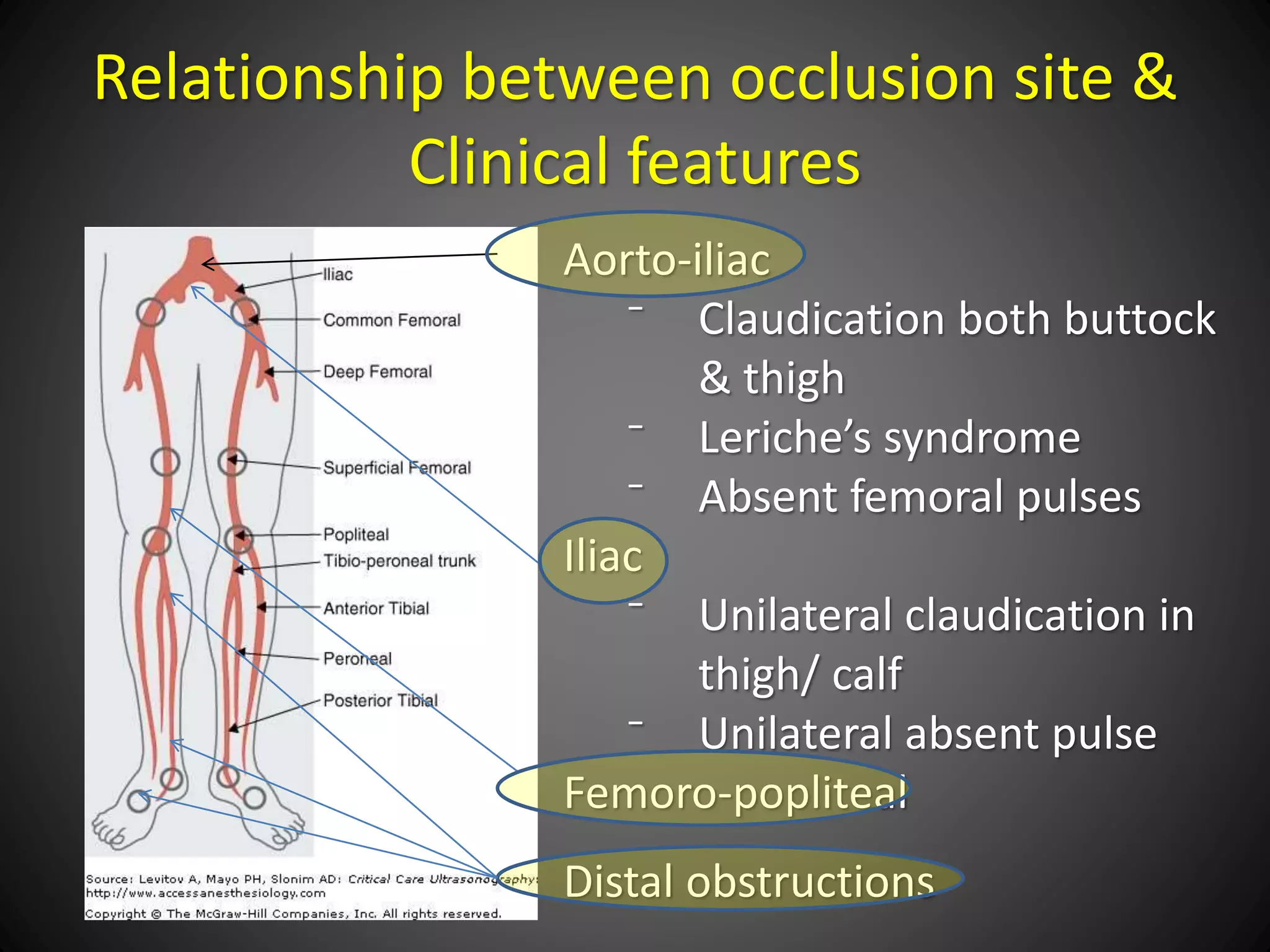
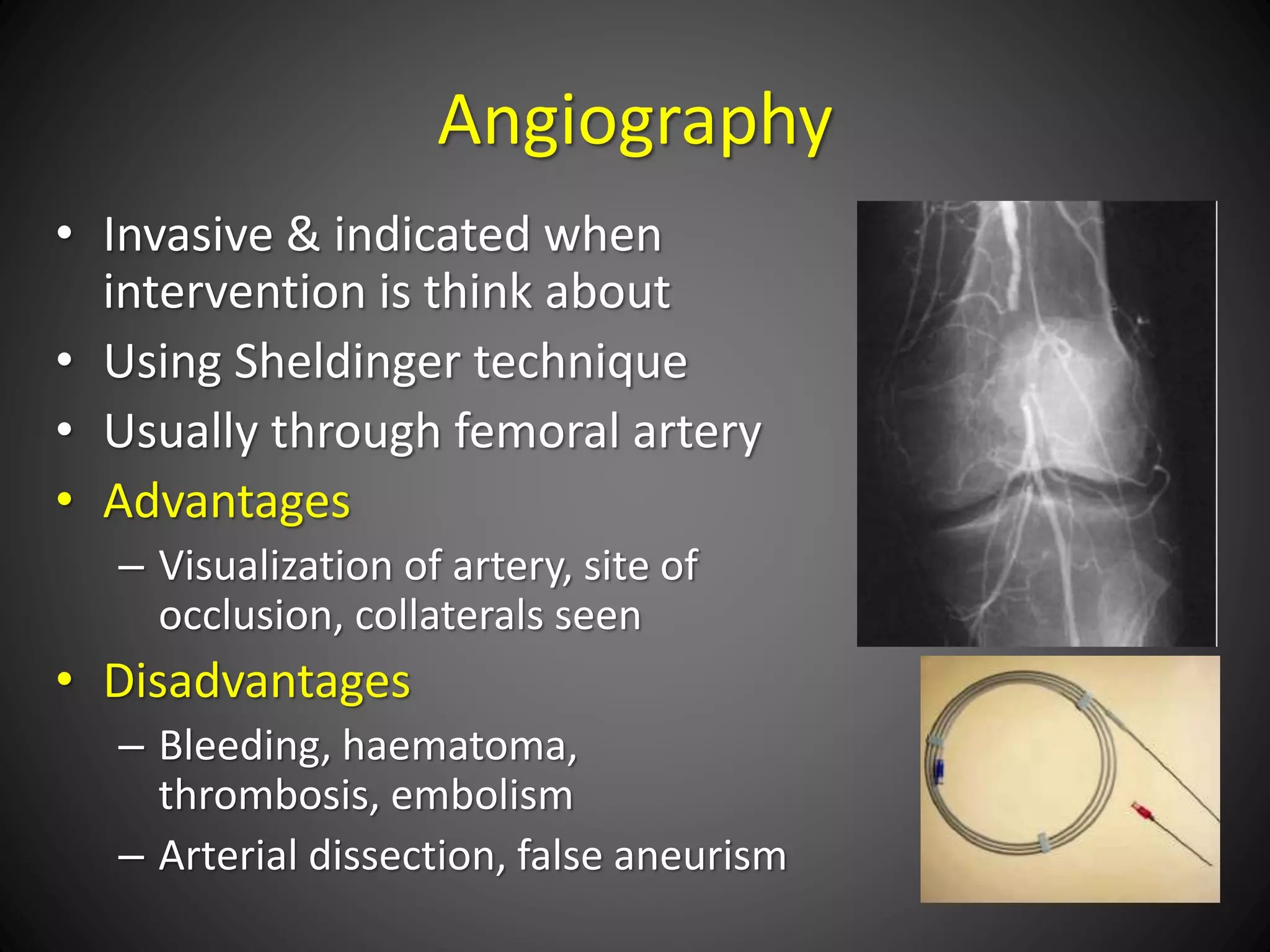
Peripheral vascular disease (PVD) refers to narrowed, blocked, or spasming blood vessels outside the heart and brain. It is commonly caused by atherosclerosis which leads to the buildup of fatty plaques in the arteries (atherosclerotic plaques). Symptoms range from mild intermittent leg pain with walking (intermittent claudication) to severe leg or foot pain at rest or skin ulcers/gangrene of the lower leg or foot. Treatment involves lifestyle changes, medications to reduce pain, plaque, or blood clotting, and potentially minimally invasive or open surgical procedures to restore blood flow if more conservative options are ineffective.