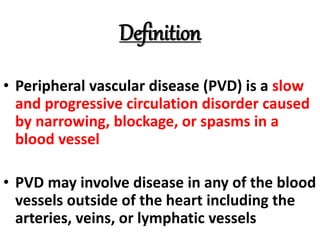
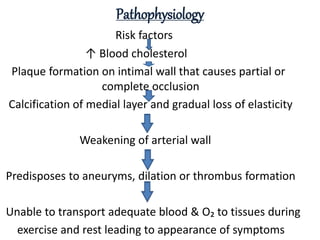
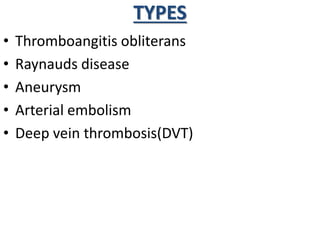
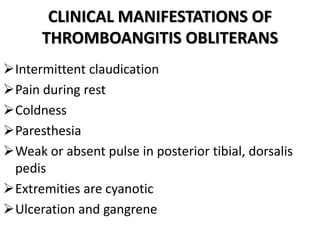
This document provides information on peripheral vascular disease (PVD). It defines PVD as a circulation disorder caused by narrowing or blockage of blood vessels outside the heart. Common risk factors include atherosclerosis, smoking, hypertension, and obesity. Symptoms vary depending on the type of PVD but may include leg pain, skin changes, and ulceration. Diagnostic tests include Doppler ultrasound, angiography, and measuring ankle-brachial index. Treatment involves lifestyle changes, medications, procedures like angioplasty or bypass surgery, and sometimes amputation for severe cases. Nursing care focuses on wound prevention, exercise, smoking cessation education, and monitoring for complications.