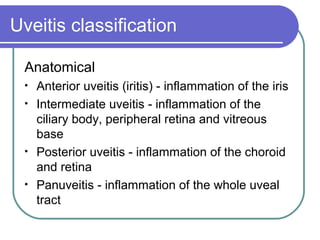
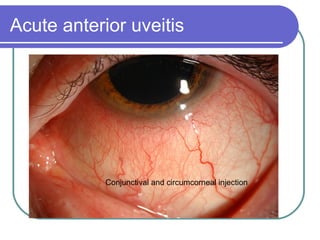
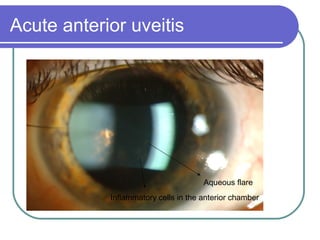
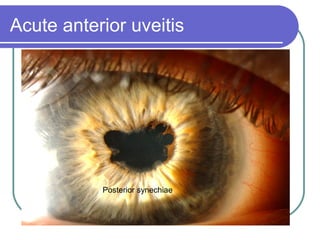
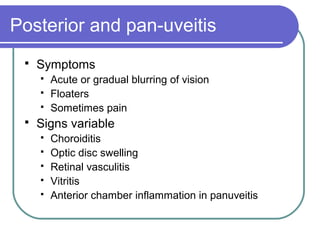
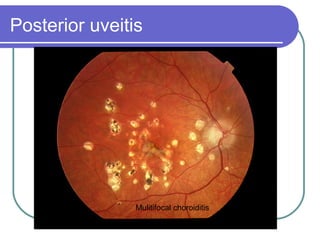
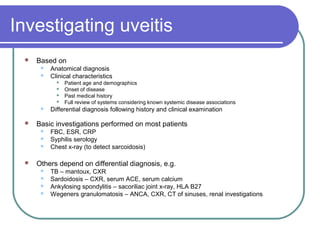
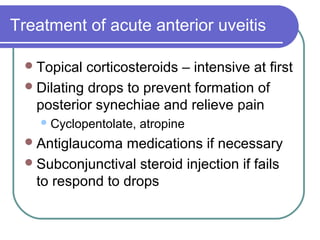
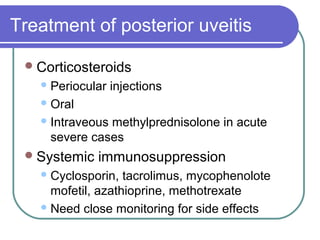
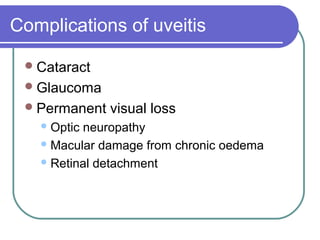
Uveitis refers to inflammation of the uveal tract of the eye. It can be classified anatomically as affecting the anterior, intermediate, or posterior segments of the eye. Common causes include autoimmune disorders, infections, and neoplasms. Symptoms and signs depend on the location and severity of inflammation. Treatment involves topical or systemic corticosteroids and immunosuppressive medications. Complications can include vision loss if uveitis is not properly treated.