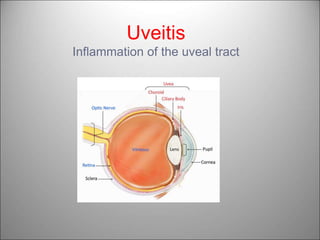
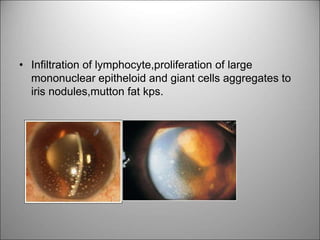
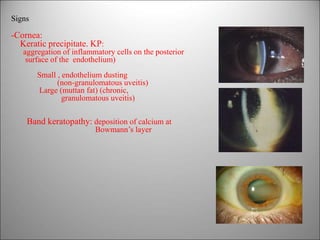
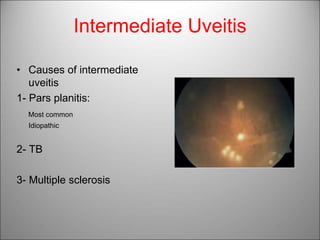
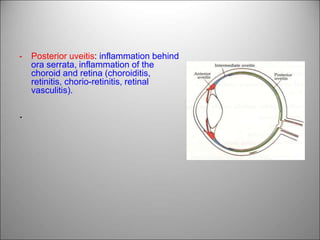
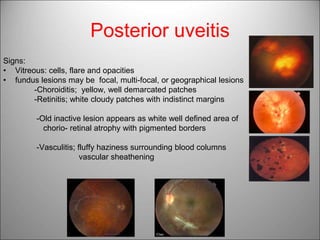
Uveitis refers to inflammation of the uveal tract of the eye. It can be caused by infections, autoimmune disorders, or malignancies. Uveitis is classified anatomically by the area of inflammation - anterior, intermediate, posterior, or panuveitis. It is also classified clinically based on duration and course. Anterior uveitis presents with pain, photophobia, redness, and blurred vision. Signs include cells and flare in the anterior chamber, keratic precipitates, and iris lesions. Intermediate uveitis affects the vitreous and peripheral retina. Posterior uveitis causes floaters and fundus lesions. Management involves identifying the etiology, using topical and systemic st