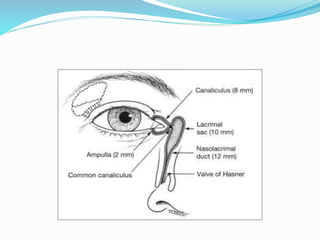
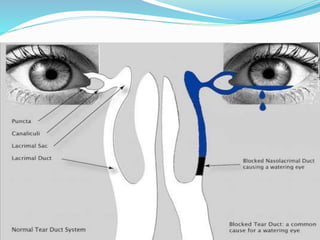
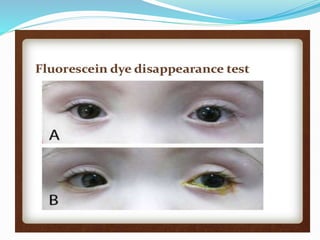
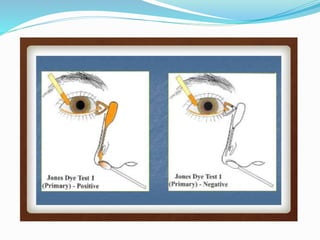
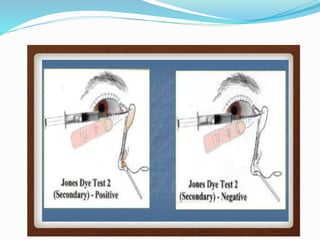
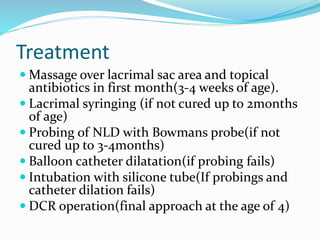
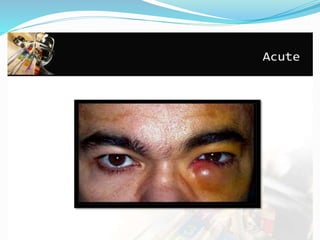
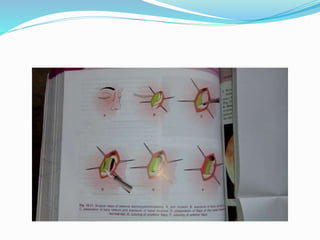
This document discusses watering eye (epiphora) and its causes including hyperlacrimation and obstruction of tear outflow. It describes various mechanical obstructions that can cause epiphora such as punctal, canalicular, lacrimal sac or nasolacrimal duct obstructions. Clinical evaluation methods are outlined. Dacryocystitis, an infection of the lacrimal sac, is discussed including its congenital and acquired forms. Congenital dacryocystitis presents in newborns with epiphora, positive regurgitation test and swelling. Acquired dacryocystitis can be chronic or acute, with chronic forms including catarrhal dacryocystitis, lacrimal