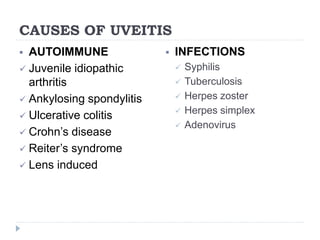
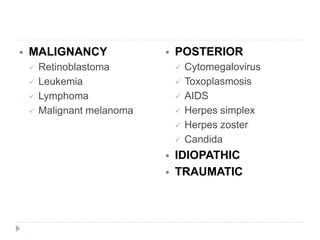
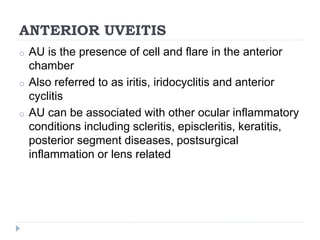
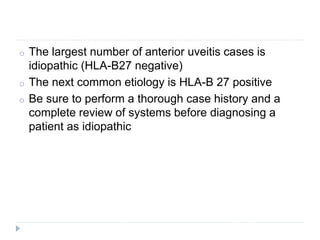
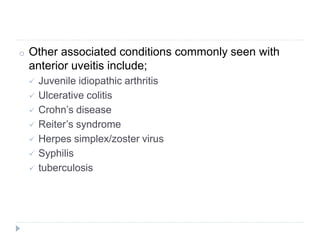
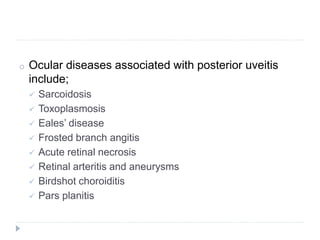
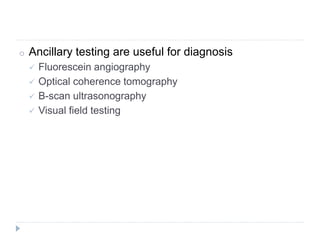
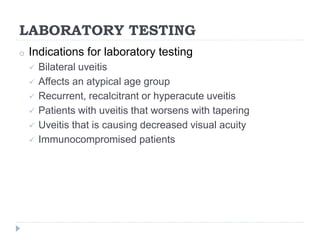
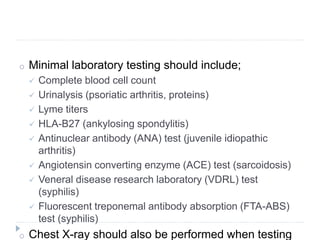
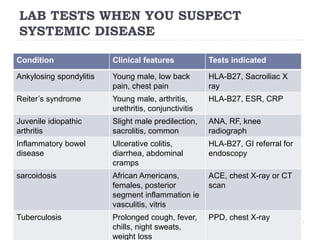
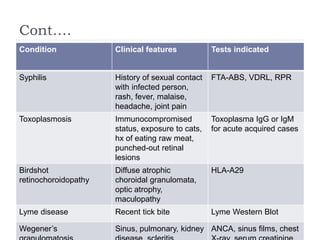
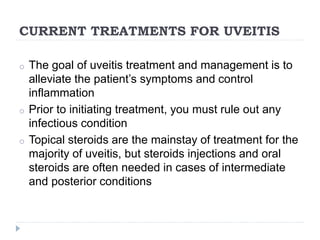
Uveitis refers to inflammation within the eye and is a leading cause of blindness. It was once considered a single disease but is now known to have various causes, including autoimmune disorders, infections, malignancy, and toxoplasmosis. A thorough evaluation including history, examination, and testing is needed to determine the extent, structures affected, underlying cause, and best treatment. Treatment involves topical steroids as first line but may require periocular injections or oral steroids depending on severity and location of inflammation. Long term management balances control of inflammation with risks of treatment side effects like increased eye pressure.