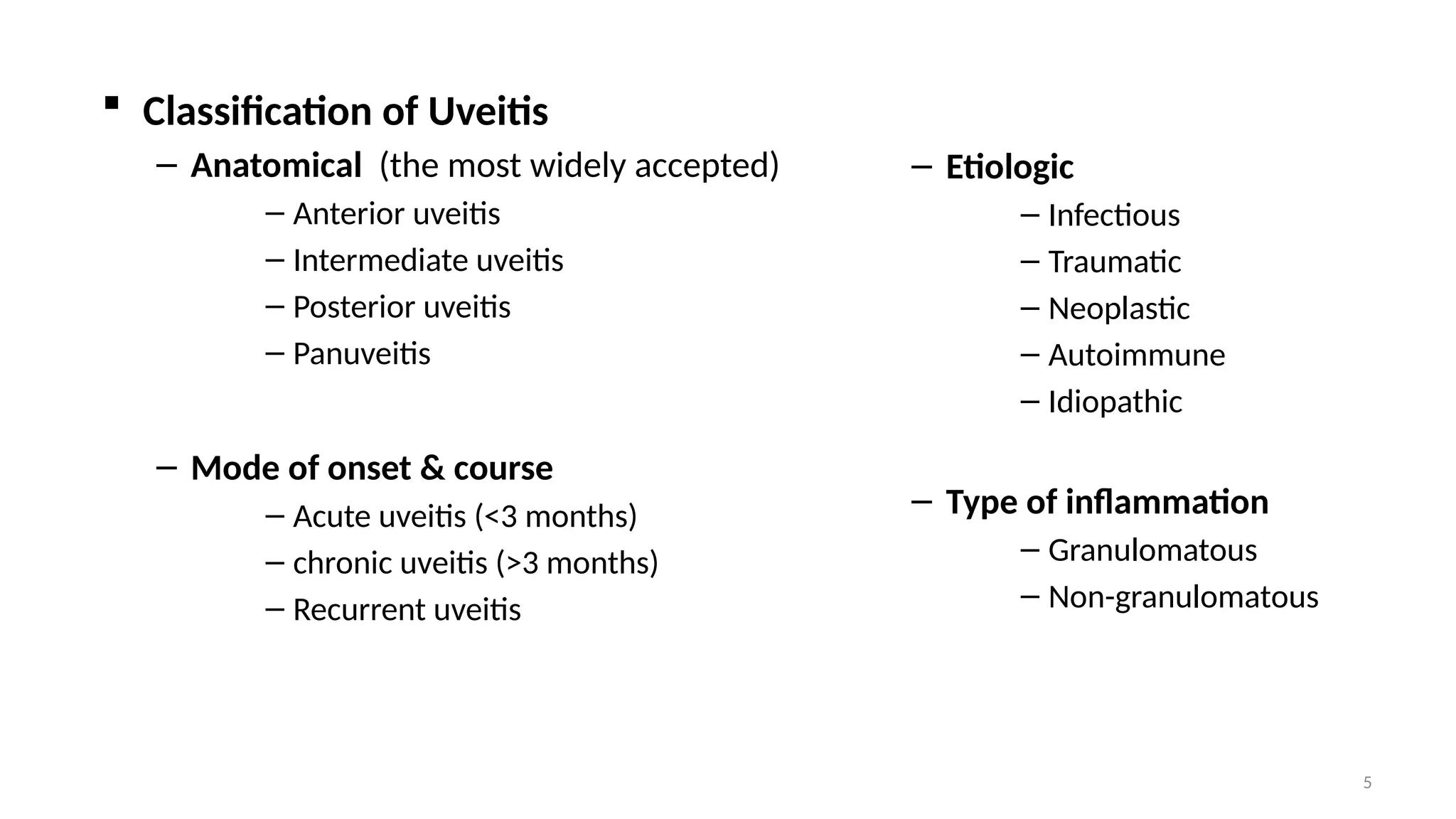
The document provides an overview of uveitis, an inflammation of the uvea categorized into anterior, intermediate, posterior, and panuveitis based on anatomical location. It discusses the causes, classifications, clinical presentations, and diagnostic approaches, emphasizing the importance of differentiating between infectious and non-infectious causes for effective treatment. Treatment options include managing underlying conditions, supportive strategies, and corticosteroid therapies tailored to the specific type of uveitis.