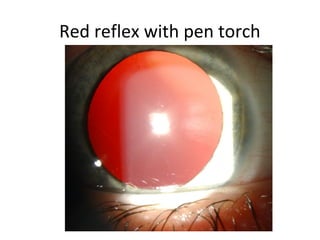
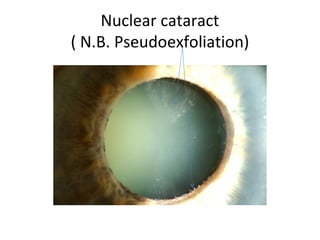
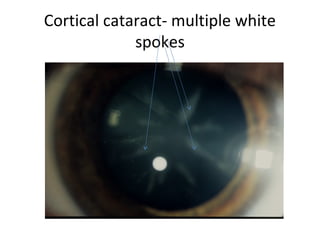
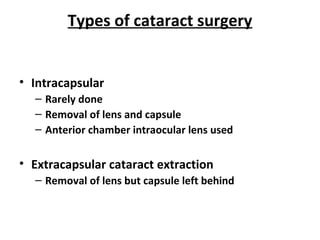
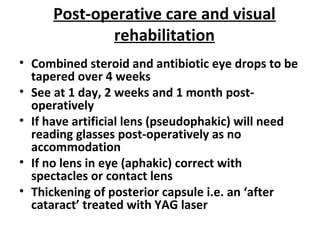
This document provides information about cataracts and cataract surgery. It defines a cataract as any opacity of the crystalline lens. It describes the anatomy of the normal lens and how it changes with age. It discusses the various types of cataracts and their causes. Symptoms include glare, reduced vision, and changes in refractive error. Examination involves evaluating the red reflex and examining the lens under a slit lamp. Treatment is typically phacoemulsification surgery, which uses ultrasound to break up and remove the cloudy lens. The cloudy lens is replaced with an intraocular lens. Post-operative care involves eye drops and follow up visits to monitor healing and vision.