1) The document discusses the anatomy, classifications, clinical features, and treatment of uveitis.
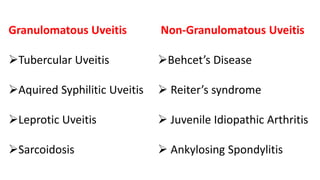
2) Uveitis refers to inflammation of the uveal tract which includes the iris, ciliary body, and choroid. It can be classified anatomically by which structure is involved - anterior, intermediate, or posterior uveitis.
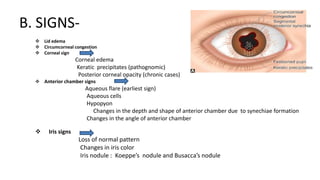
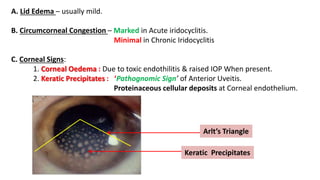
3) Clinical signs of anterior uveitis/iridocyclitis include pain, redness, photophobia, blurred vision, and keratic precipitates on the cornea. Treatment involves cycloplegic eye drops to relieve inflammation and prevent complications.